Neonatology
Session: Neonatal Follow-up 1
498 - Parent and Stakeholder Perspectives on Barriers and Facilitators to Care for Infants with Bronchopulmonary Dysplasia After NICU Discharge
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 498
Publication Number: 498.1190
Publication Number: 498.1190

Joanne Lagatta, MD (she/her/hers)
Professor
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
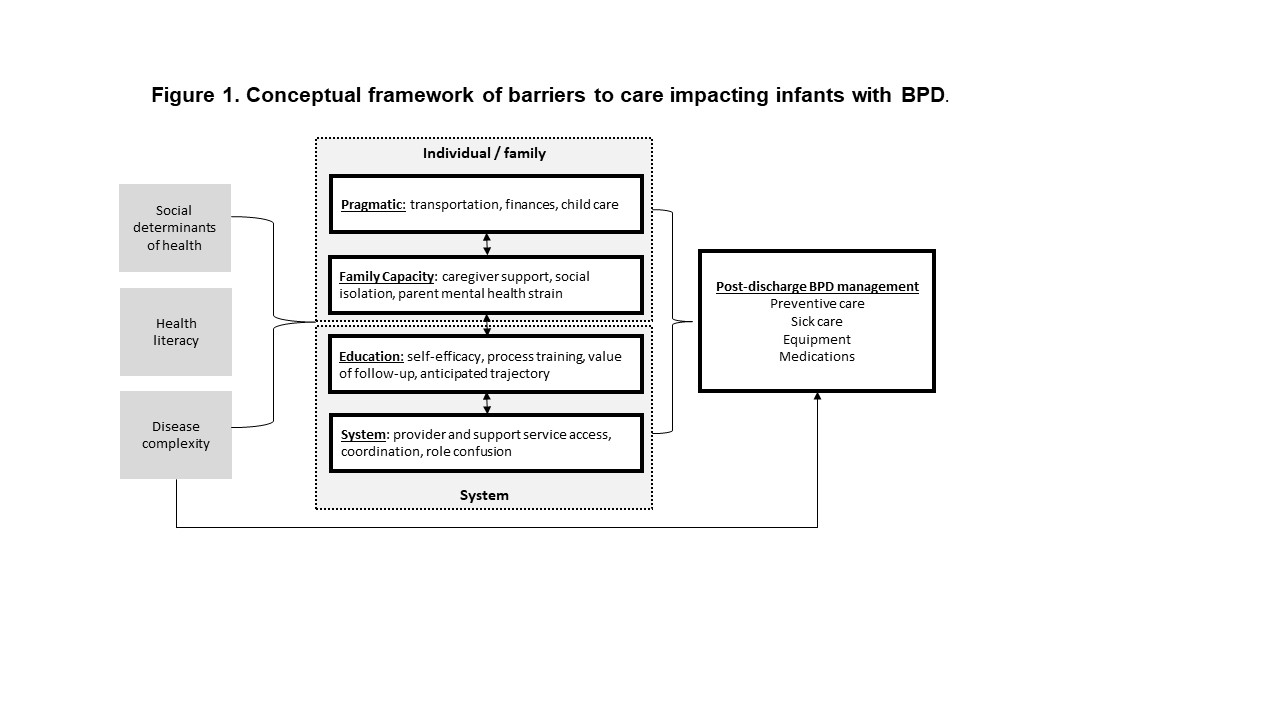
Background: Preterm infants with bronchopulmonary dysplasia (BPD) receive complex multidisciplinary supports to improve health outcomes after neonatal intensive care unit (NICU) discharge. However, complex follow-up care can be challenging for families. Socioeconomic and racial disparities that increase risk of preterm birth likely also impact discharge preparation and use of follow-up care. A framework to understand barriers and facilitators to follow-up care for infants with BPD could help understand the impact of interventions in this population.
Objective: To understand barriers and facilitators to follow-up care for infants with BPD.
Design/Methods: Qualitative study of parents and clinical stakeholders caring for infants with BPD after NICU discharge. The interview guide was developed by a mother of a former 23-week preterm infant, neonatologist, pulmonologist, nurse, and qualitative researcher. Purposive sampling obtained a heterogenous sociodemographic and professional cohort. Subjects discussed their experience with BPD, barriers to care, caregiver quality of life and health education. Interviews were audio-recorded, transcribed and coded. Thematic analysis was used.
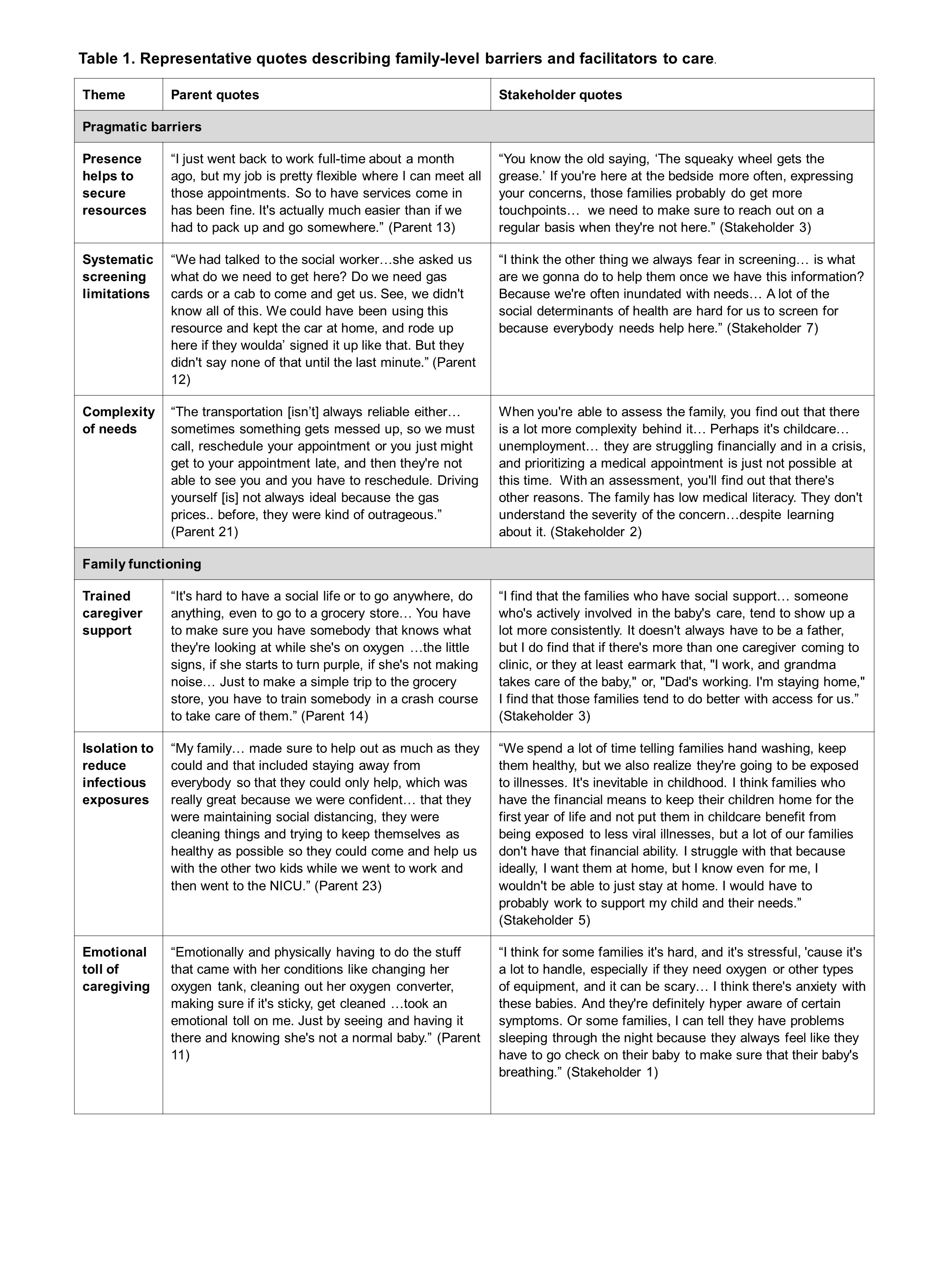
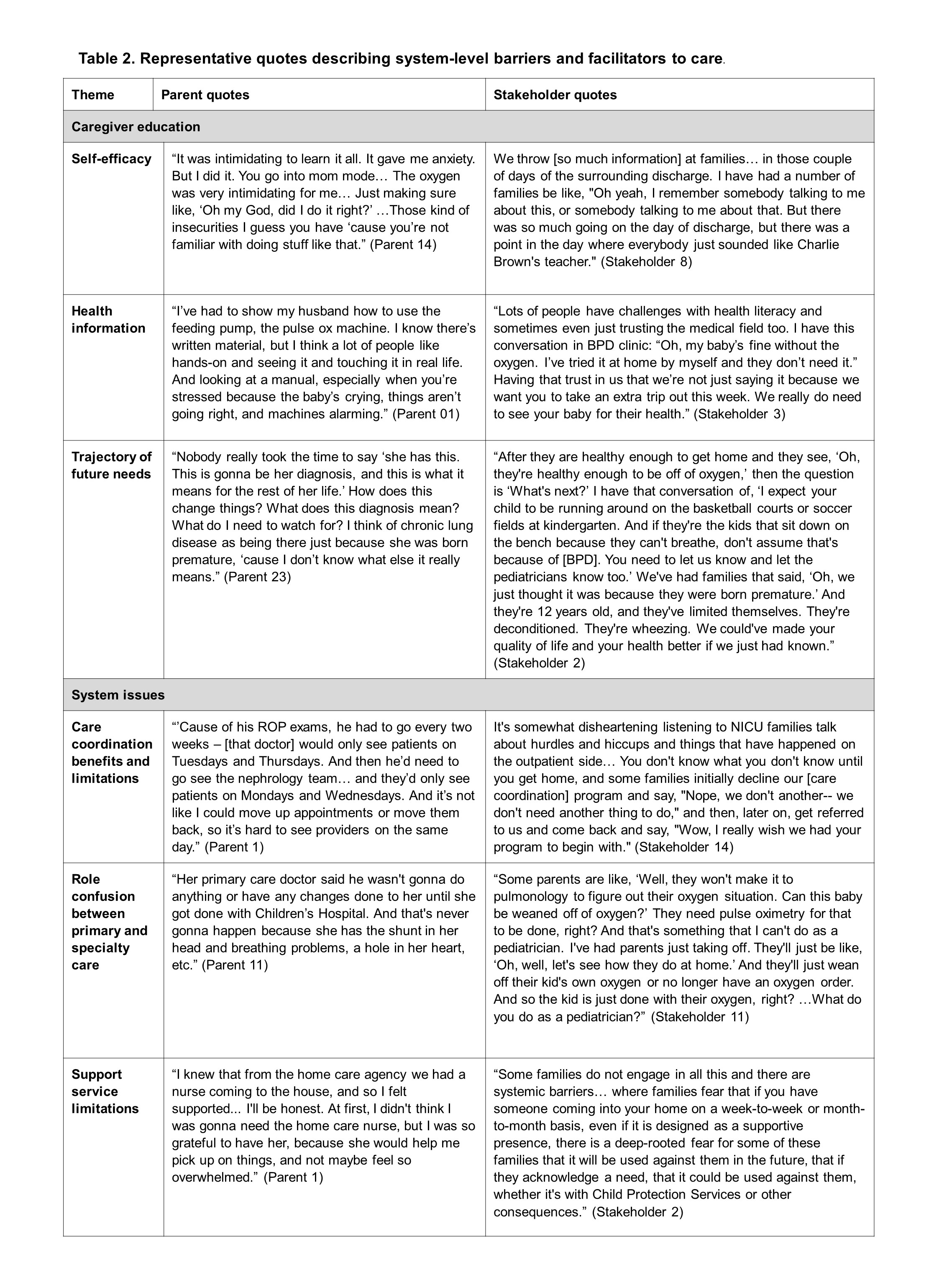
Results: Eighteen parents and 20 stakeholders completed interviews. Parents represented a range of education, income, race and ethnicity; stakeholders represented specialty and primary care, social work, care coordination and community services. Two primary themes of family- and system-level barriers and facilitators were identified. Family themes (Table 1) included pragmatic barriers such as transportation, finances, and childcare, and family capacity barriers such as caregiver support (trained second caregiver), social isolation (minimize infectious exposure), and parent mental health (emotional toll of caregiving). System level themes (Table 2) included educational issues such as self-efficacy, understanding of expected patient trajectories, and the value of follow-up care; system barriers and facilitators included provider and support service access, care coordination, and role confusion (pediatrician vs. specialists). Constructs of social determinants of health, health literacy and disease complexity connected these themes (Figure 1). For example, financial barriers limit in-person communication which limits second-caregiver training and family education.
Conclusion(s): Convergence by families and stakeholders on individual and system-level barriers and facilitators inform a conceptual framework for measurement and quality improvement initiative to improve NICU to home transitions for complex infants such as those with BPD.