Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
377 - Making it Easy to Say Yes: Using a Quality Improvement Approach to Boost Immunization Rates and Examine Equity in an Adolescent Medicine Practice
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 377
Publication Number: 377.2235
Publication Number: 377.2235
- JB
Josh Borus, MD. MPH (he/him/his)
Physician
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Vaccinations protect against preventable harmful diseases. Complete vaccine records enable adolescents to access opportunities including school, work, and sports.
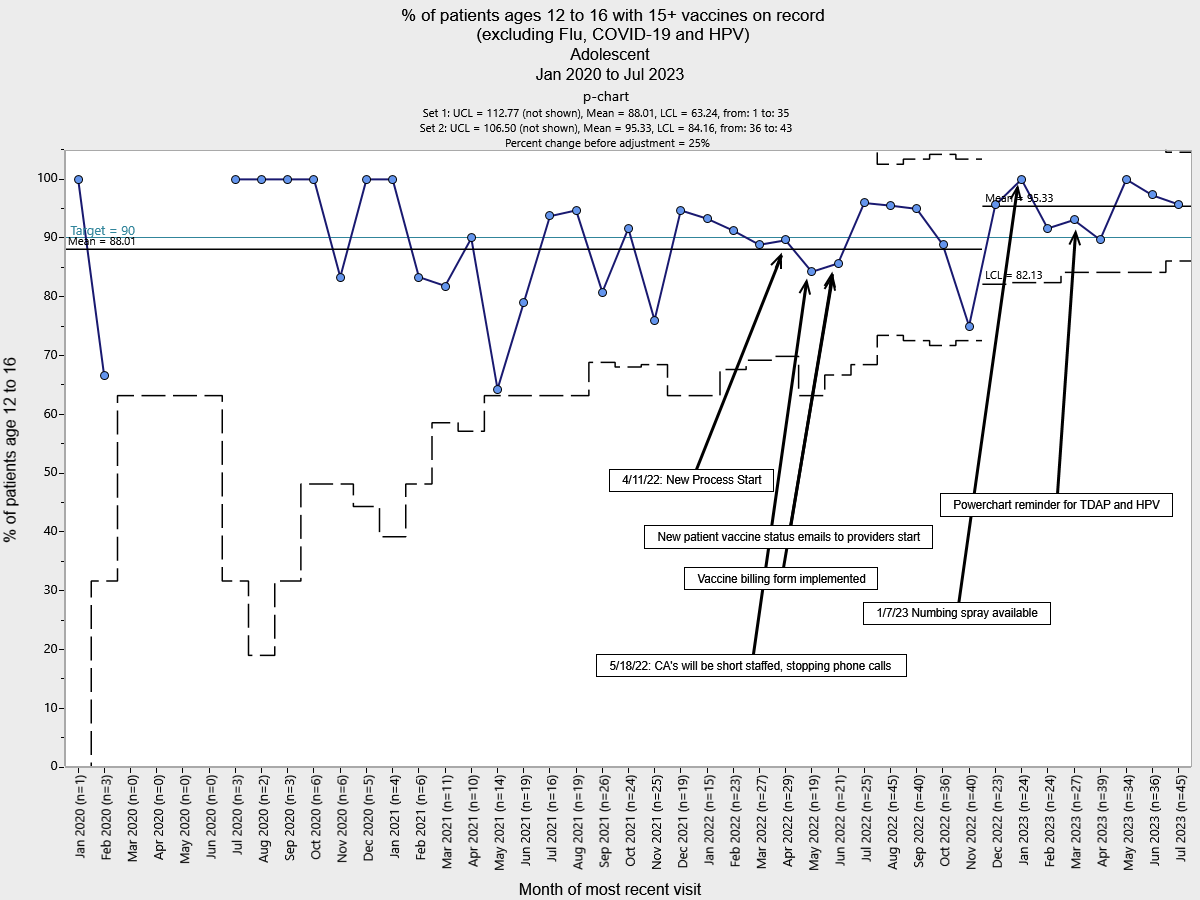
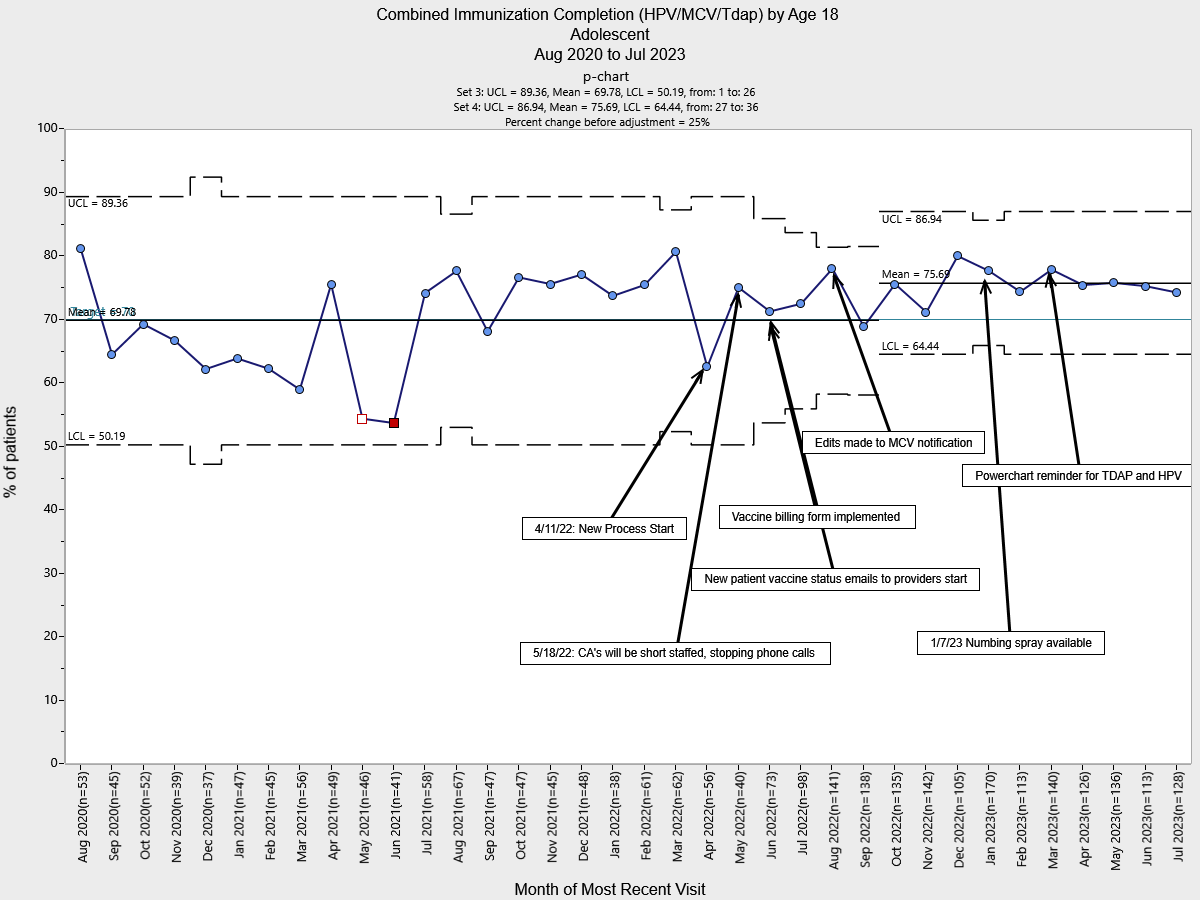
Objective: We sought to: 1) increase the % of patients with a complete vaccination record from 88% to 95%, 2) increase the % of patients who are up to date on their meningococcal (MCV), human papillomavirus (HPV), and Tetanus, Diphtheria, and Pertussis (Tdap) vaccinations from 70% to 80%, and 3) ensure that our efforts led to more equitable care.
Design/Methods: We launched a quality improvement (QI) project involving the key process stakeholders. Using QI tools we found that the primary drivers to meet our goal were: 1) documentation of vaccines from outside clinics, 2) provider reminders of vaccine status at all visits, and 3) patient acceptability of vaccines.
The first Plan-Do-Study-Act (PDSA) cycle was a process for nurses to import existing vaccine records from the Massachusetts Immunization Information System and make outreach to new patients/families to obtain missing records. We implemented semi-automated alerts in the Electronic Medical Record (EMR) to alert providers when patients are overdue for immunizations. Finally, all patients are now offered numbing spray to mitigate vaccine hesitancy.
Analytical methods were statistical process control p-chart analysis. We explored rates of vaccine completion by race/ethnicity and payor status.
Results: Special cause variation was demonstrated with a shift in the % of patients with a complete vaccination record from 88% to 95%. Similarly, there was a mean shift for the combined HPV/MCV/Tdap completion rate from 70% to 76%.
Racial disparity analysis for the HPV/MCV/Tdap measure showed that pre-intervention, the highest performing group was Black patients while post-intervention, the reference group shifted to Hispanic patients. Almost all subgroups improved equally and there was a statistically significant improvement observed for the whole population (p < 0.001). When comparing publicly versus privately insured patients, there were no disparities found before or after interventions. There was a statistically significant improvement for publicly insured patients (p < 0.001).
Conclusion(s): The bundled intervention approach including outreach to patients, patient education, and technology fixes contributed to increases in vaccine documentation and administration rates. Next steps include collaborating with Information Technology representatives to fully automate the EMR alert. We will further investigate racial disparities within our population and launch interventions as needed.
.png)