Neonatology
Session: Neonatal Neurology 7: Neurodevelopment
620 - Neonatal neurobehavior predicts NOWS severity prior to treatment
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 620
Publication Number: 620.1123
Publication Number: 620.1123
- EC
Elisabeth Conradt, PhD (she/her/hers)
Associate professor
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: Newborns exposed to opioids in utero are at risk for Neonatal Opioid Withdrawal Syndrome (NOWS). To guide treatment of NOWS, clinicians use observational diagnostic tools. However, concerns about the standardization and lack of reliability of these tools have been raised. The absence of early, reliable, and valid diagnostic measures of NOWS may limit medical professionals’ ability to provide optimal care to opioid- exposed newborns.
Objective: We examined whether NOWS risk could be detected as early as 24 hours after birth (prior to most signs of withdrawal) using a standardized neurobehavioral assessment to predict NOWS severity throughout the newborns’ hospital stay.
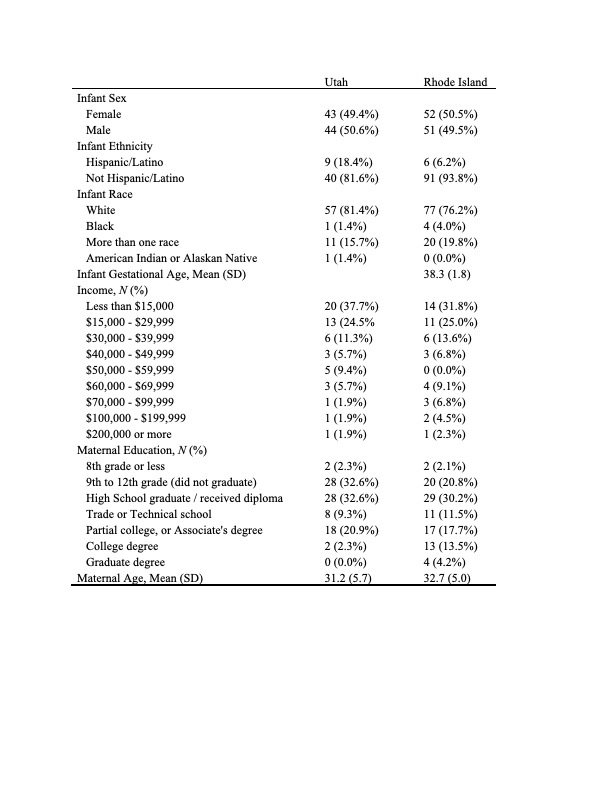
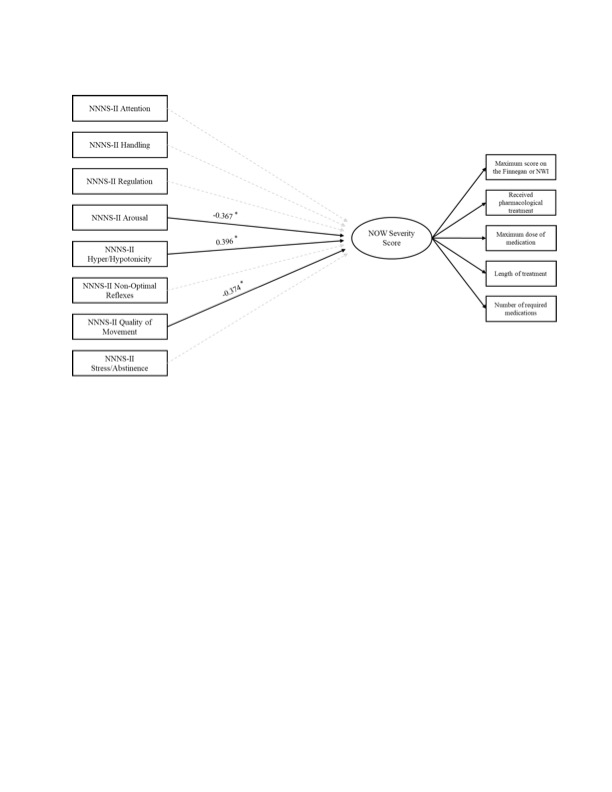
Design/Methods: We enrolled 193 newborns with prenatal opioid exposure at birth. NOWS diagnosis in this multisite study was assessed using the Modified Finnegan Neonatal Abstinence Scoring Tool or the Neonatal Withdrawal Inventory (NWI). NOWS severity was measured using the indicators in Figure 1. Neonatal neurobehavior was assessed shortly after birth (M=1.43 days old, SD = 1.62) by trained examiners using the NeoNatal Neurobehavioral Scale (NNNS-II). Structural equation modeling was conducted in R (lavaan package) with maximum likelihood estimation.
Results: Confirmatory factor analysis tested a one-factor model of NOWS Severity Score, and acceptable fit was achieved, χ2(5) = 10.183, p = .07, RMSEA = .079, CFI = .992. The five factor loadings were substantial, statistically significant, and the range was relatively narrow (standardized λs = 0.692 - 0.971, all ps < 0.01). We estimated a full structural model to examine the relations between the NNNS-II subscales and the NOWS Severity Score latent factor, and acceptable model fit was achieved, χ2(41) = 51.118, p = .13, RMSEA = .071, CFI = .967 (Figure 1). The significant predictors of NOWS Severity Score include NNNS-II Hyper/Hypotonicity, Quality of Movement, and Arousal. Poor quality of movement was associated with increased risk for a NOWS severity score in the top 25th percentile (aRR, 4.1; 95% CI, 1.55-14.17). We found that dysregulated newborn neurobehavior, measured as early as 24 hours after birth, predicted NOWS severity throughout the newborns’ hospital stay (M = 10.16 days; SD = 7.37). Newborns with more tone abnormalities (i.e., either hyper- or hypotonic), lower quality of movement, and less arousal had higher NOWS severity scores.
Conclusion(s): Standardized, evidence-based interventions are needed to predict risk for NOWS diagnosis and NOWS severity. These findings indicate that NOWS severity risk can be detected with early newborn neurobehavioral assessment.