Neonatology
Session: Neonatal Pulmonology - Clinical Science 4: Clinical Practice Questions, Going Home
571 - Premedication for Neonatal Rapid Sequence Intubation: A Network Meta-analysis
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 571
Publication Number: 571.2828
Publication Number: 571.2828
.jpg)
Dwayne D. Mascarenhas, MD, DM (he/him/his)
Clinical Fellow
University of Toronto
Toronto, Ontario, Canada
Presenting Author(s)
Background: Endotracheal intubation is the most common procedure among neonates and procedural failure or difficulty is associated with increased mortality and morbidity. Premedication, using one or a combination of a short-acting opioid (SAO), long-acting opioid (LAO), and/or sedative-hypnotic (SH), with or without a neuromuscular blocker (NMB), is often administered to improve intubation conditions and success. However, the optimum premedication regimen remains unknown, as a limited number of clinical trials have each investigated regimens with different pharmacological agents.
Objective: To systematically review and conduct a network meta-analysis of premedication regimens for endotracheal intubation among neonates.
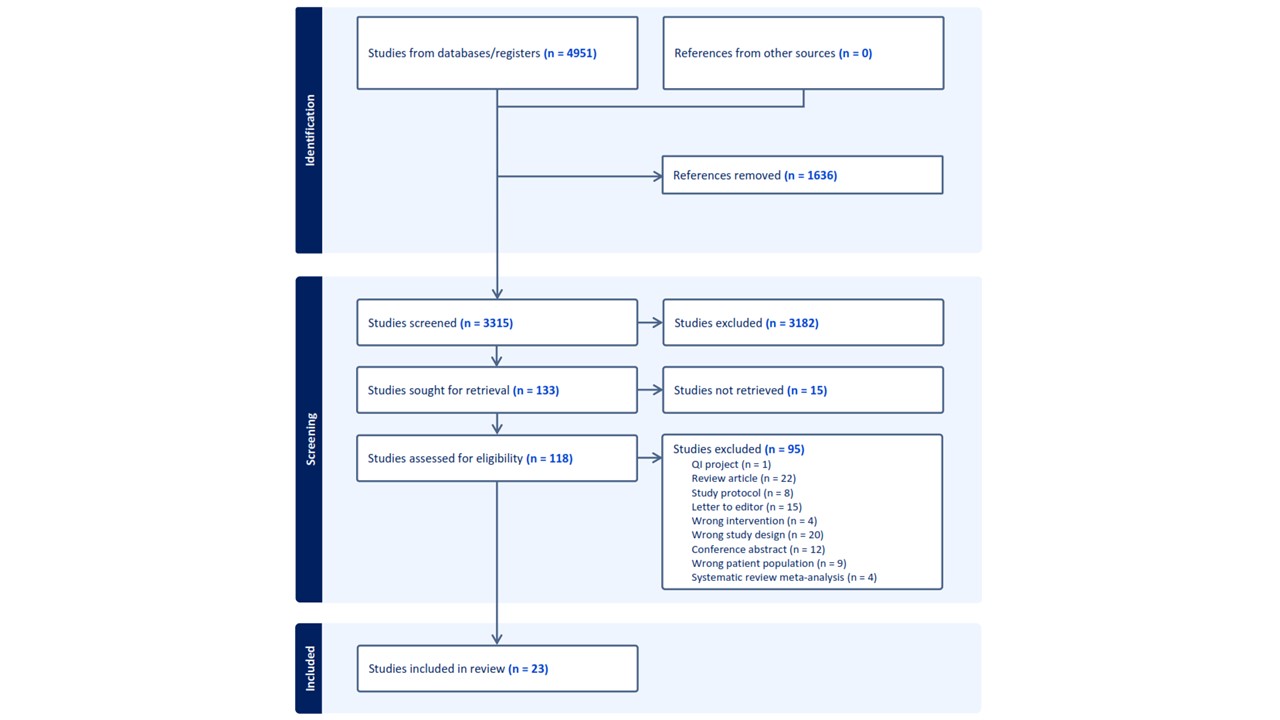
Design/Methods: PubMed, Embase, CINAHL, and Cochrane CENTRAL databases were searched from inception until May 23, 2023 for randomized clinical trials (RCTs) comparing premedication regimens for non-emergent endotracheal intubation among neonates. To be able to draw generalizable conclusions on the different premedication regimens, pharmacological agents were grouped into nodes by medication class [SAO: fentanyl, remifentanil, alfentanil; LAO: morphine, meperidine; SH: midazolam, propofol, thiopental; NMB: mivacurium, atracurium, pancuronium, succinylcholine) Data were extracted for random-effects network meta-analysis to estimate the relative risk [RR] and 95% confidence intervals [CI]), and surface under the cumulative ranking (SUCRA) curve value. The primary outcome was success at first intubation attempt. The secondary outcome was significant procedural hypoxemia (SpO2 < 80%). Risk of bias was assessed using the Cochrane ROB-2 tool. Confidence In NEtwork Meta-Analysis software was used to assess the certainty of evidence (CoE) and grade outcomes.
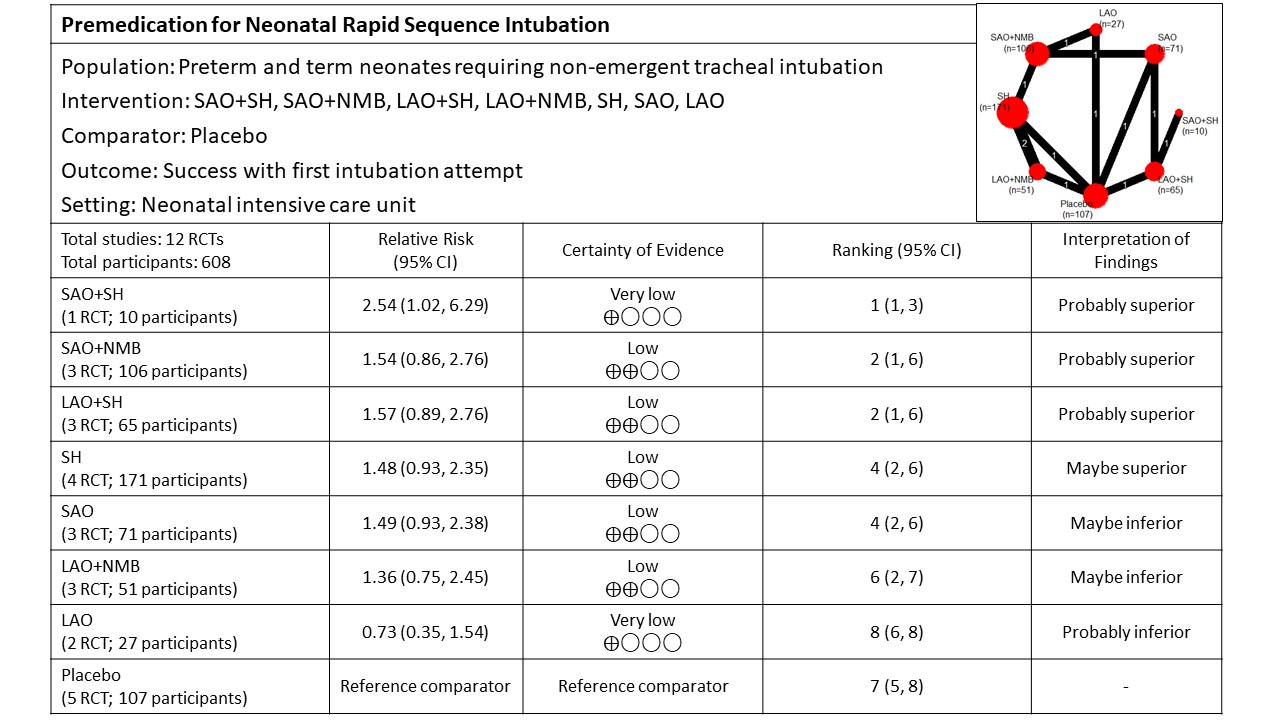
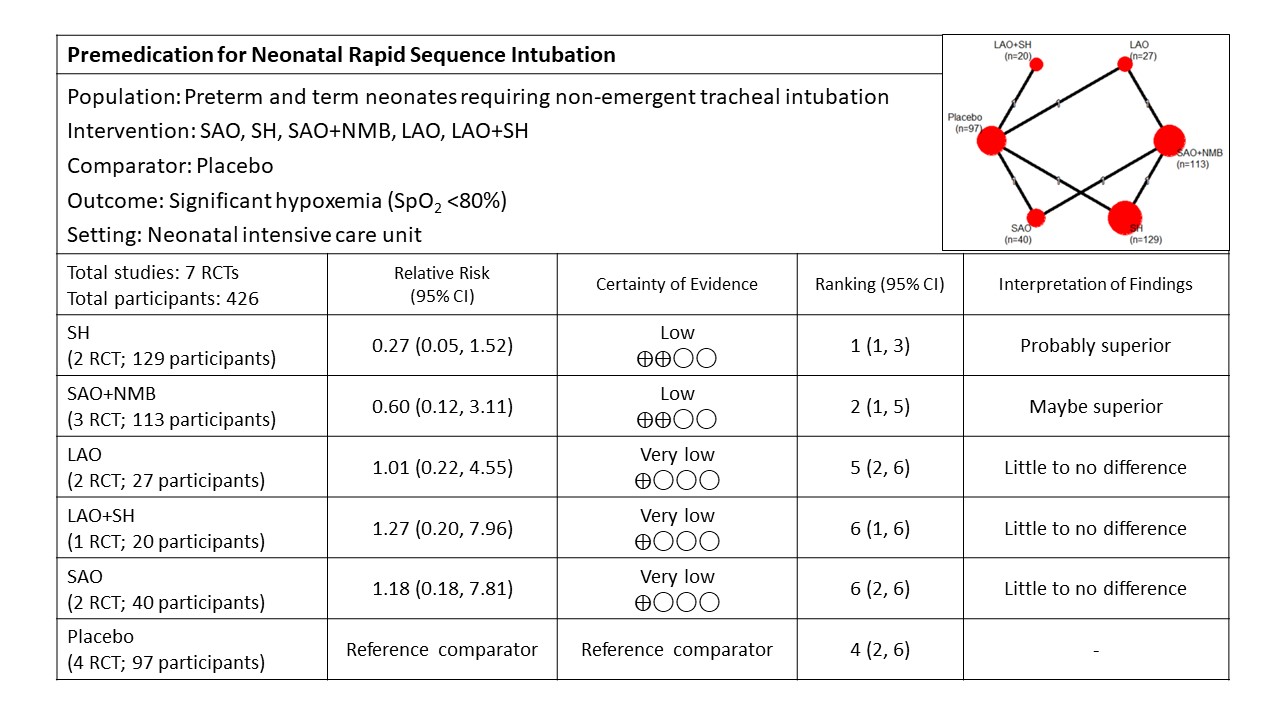
Results: Twenty-three RCTs enrolled 931 neonates (Figure 1). Pooled analysis identified that premedication with SAO+SH probably results in improved intubation success (network RR 2.54 [vs. placebo], 95% CI 1.02, 6.29; median rank 1, 95% CI 1-3; very low-certainty; Figure 2). There were no significant differences among premedication regimens with respect to the risk for significant hypoxemia during intubation (Figure 3).
Conclusion(s): Very low-certainty evidence suggests that a combination of a sedative-hypnotic and short-acting opioid probably results in a higher likelihood of successful intubation. Adequately powered well-designed RCTs in the neonatal population are required to corroborate these findings.