Immunizations/Delivery
Session: Immunizations/Delivery 1
45 - Factors Associated with COVID-19 Vaccine Uptake Among Children in a Regional Federally Qualified Health System
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 45
Publication Number: 45.1163
Publication Number: 45.1163
.jpg)
Sameer J. Patel, MD, MPH (he/him/his)
Associate Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, IL, Illinois, United States
Presenting Author(s)
Background: Children with lower socioeconomic status and from minoritized groups experience disparities in vaccine uptake. There is limited data on factors associated with COVID-19 vaccination among low-income children with chronic health conditions.
Objective: We evaluated factors associated with COVID-19 vaccination in children receiving primary care at a federally qualified health center (FQHC).
Design/Methods: We retrospectively evaluated vaccine uptake in children aged 7 months to 18 years who received primary care in a regional FQHC system and had ≥1 encounter at a large, academic children’s hospital. Multivariable logistic regression identified factors associated with receipt of 1) at least one dose of COVID-19 vaccine and 2) bivalent COVID-19 booster after completion of primary series. Additionally, we identified factors associated with time to receipt of bivalent COVID-19 booster after first availability. Covariates included age (0.5 to 4, 5-11, 12-15, and 16+ years), sex, race/ethnicity, primary language, childhood opportunity index (COI), and chronic conditions.
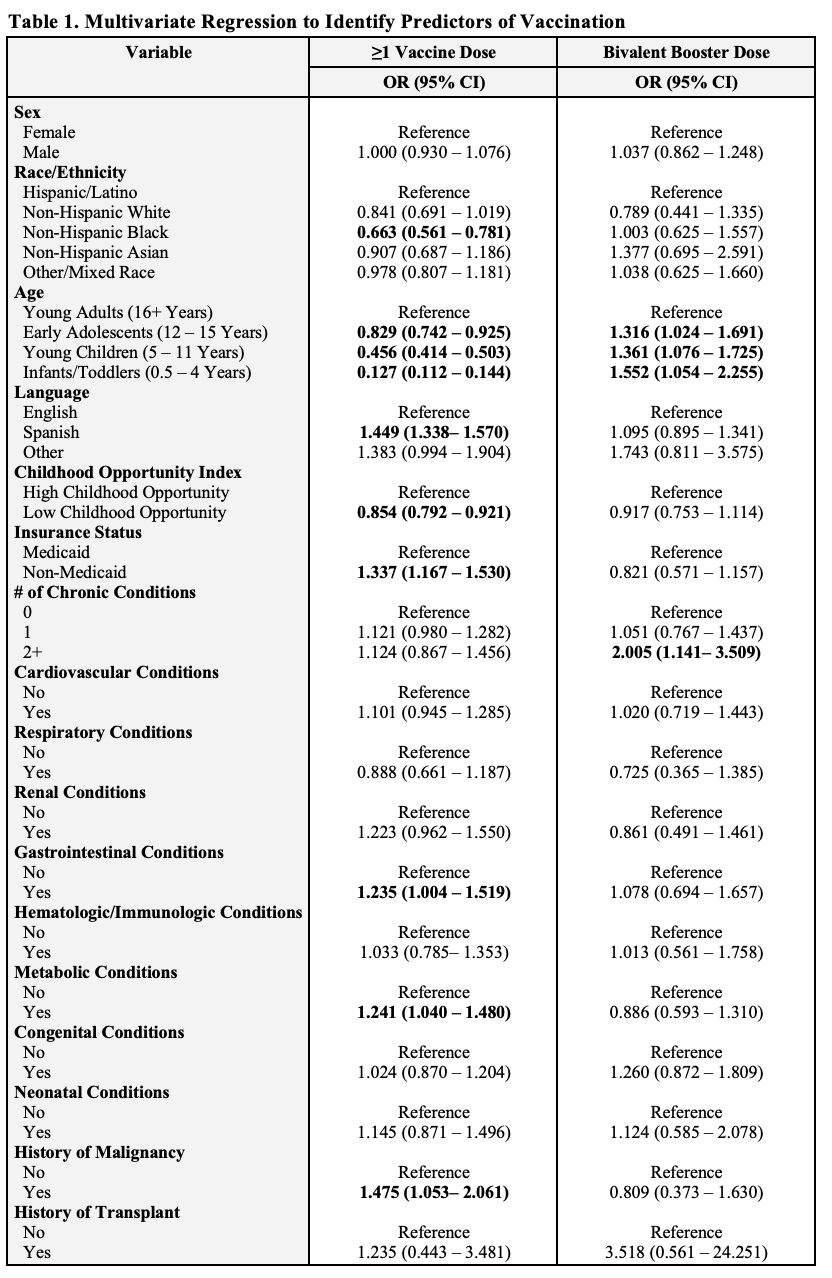
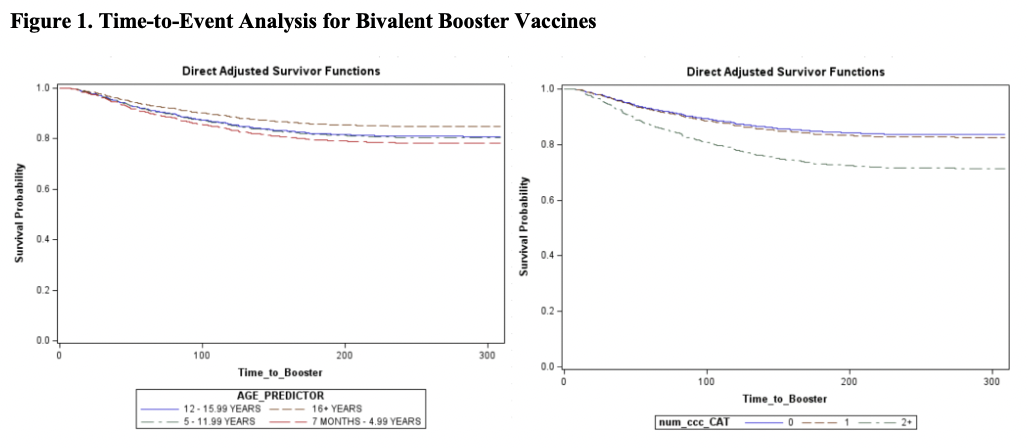
Results: Of 17,878 patients, 4,606 (25.8%) received ≥1 vaccine dose. A total of 2,573 patients completed the primary vaccine series (14.4%), while only 638 (3.6%) received both the primary series and bivalent booster. As shown in Table 1, decreased likelihood of receipt of COVID-19 vaccine was associated with age 6 months to 4 years (OR 0.127, reference 16+ years), black race (OR 0.663, reference Hispanic), and very low COI (0.854). Increased uptake was associated with the presence of metabolic condition (OR 1.241), gastrointestinal condition (OR 1.235), malignancy (OR 1.475), or non-Medicaid insurance status (1.337). As outlined in Table 2, increased likelihood of COVID-19 booster vaccination was associated with younger age and 2+ chronic conditions (OR 2.005). As visualized in Figure 1, the fastest time to receive of COVID-19 booster was associated with age 6 months to 4 years (HR 1.502), followed by those aged 5 to 11 years (HR 1.326), and 12 to 16 years (HR 1.293). Additionally, 2+ chronic conditions was associated with faster vaccination (HR 1.905).
Conclusion(s): In children from families with lower socioeconomic status, disparities in vaccination included COI, Black race, Medicaid insurance, and younger age. Our subgroup analysis found once initially vaccinated, children perceived to be more vulnerable (younger aged, with multiple chronic conditions) receive booster doses quicker.