Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 2
466 - Transparency in Compensation: Empowering the Women in Neonatology
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 466
Publication Number: 466.2805
Publication Number: 466.2805

Lindsay Johnston, MD, MEd (she/her/hers)
Associate Professor
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Women and other traditionally minoritized populations may feel less empowered to advocate for themselves during negotiations and less aware of important benchmarks when considering job opportunities. Transparency in faculty compensation, clinical hours, overtime, and coverage is necessary for both benchmarking and individual negotiations.
Objective: To create a transparent data benchmark for faculty compensation across a variety of US Neonatology practices focusing on female identifying faculty.
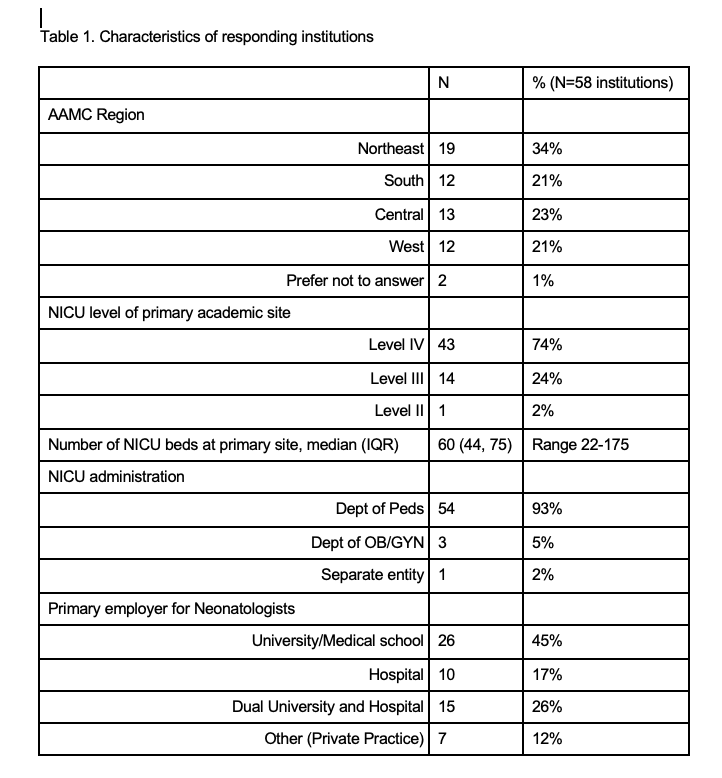
Design/Methods: Female identifying faculty in AAP’s Section on Neonatal-Perinatal Medicine’s Women in Neonatology group were asked to participate in an electronic survey on their division’s requirements for clinical hours, compensation and coverage for overtime/ backup call, salary benchmarking, and relative value unit (RVU) targets. Responses were consolidated to ensure 1 complete record per unique division.
Results: 151 respondents provided information for 58 unique neonatology divisions, the majority of which are academic (table 1). Most programs have an institutional expectation for hours worked to meet a definition of full time (n=44, 76%). For programs that use total clinical hours and have transparency in that number (n=13), the median expected clinical hours for 1.0 cFTE is 1800 hours (IQR 1656, 1944) annually. For programs that use weeks on service and have transparency in that number (n=19), the median number of weeks is 22 (IQR 19, 22) annually. The majority of the programs with in-house call include these hours towards FTE, with compensation in base-salary (n=33, 75%). Only half of groups (n=31, 53%) compensate faculty for “overtime” work (ie, clinical time above the contracted time). The reported hourly pay rate for overtime is a median of $135/hour (IQR $100, 150). Half of groups require participation in a formal back-up system (n=31, 55%), with the majority not providing compensation for backup call (n=21, 68%). Some groups reported a clear salary benchmark, most commonly based upon the Association of American Medical Colleges (AAMC) regional (n=10, 40%) or national data (n=5, 20%). A minority of programs have specific RVU target percentiles for their clinical work (n=14, 24%). Although most respondents could not define these targets, those with specified RVU ranges varied from the 50-75 percentile.
Conclusion(s): This information provides a valuable starting point for Neonatologists to benchmark their salary and clinical time allocation, and potentially negotiate for improved compensation and coverage.