Neonatology
Session: Neonatal General 3: Maternal and Fetal Medicine
91 - Neonatal Outcomes of Neonates Born to Mothers with Intrahepatic Cholestasis of Pregnancy in a Multiethnic Community Hospital
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 91
Publication Number: 91.531
Publication Number: 91.531
- NN
Neelam Neupane, MBBS (she/her/hers)
Pediatric resident
Flushing Hospital Medical Center
Flushing, New York, United States
Presenting Author(s)
Background: Intrahepatic cholestasis of pregnancy (ICP) is a common pregnancy related liver disease associated with increased risk of adverse neonatal outcomes. Clinically, ICP is characterized by pruritus without a rash. Biochemically, bile acids and serum aminotransferases are elevated in the late second to early third trimesters which rapidly resolve after delivery. There are limited data on neonatal outcomes for infants of mothers with ICP in a multiethnic population.
Objective: To explore outcomes of neonates born to mothers with ICP.
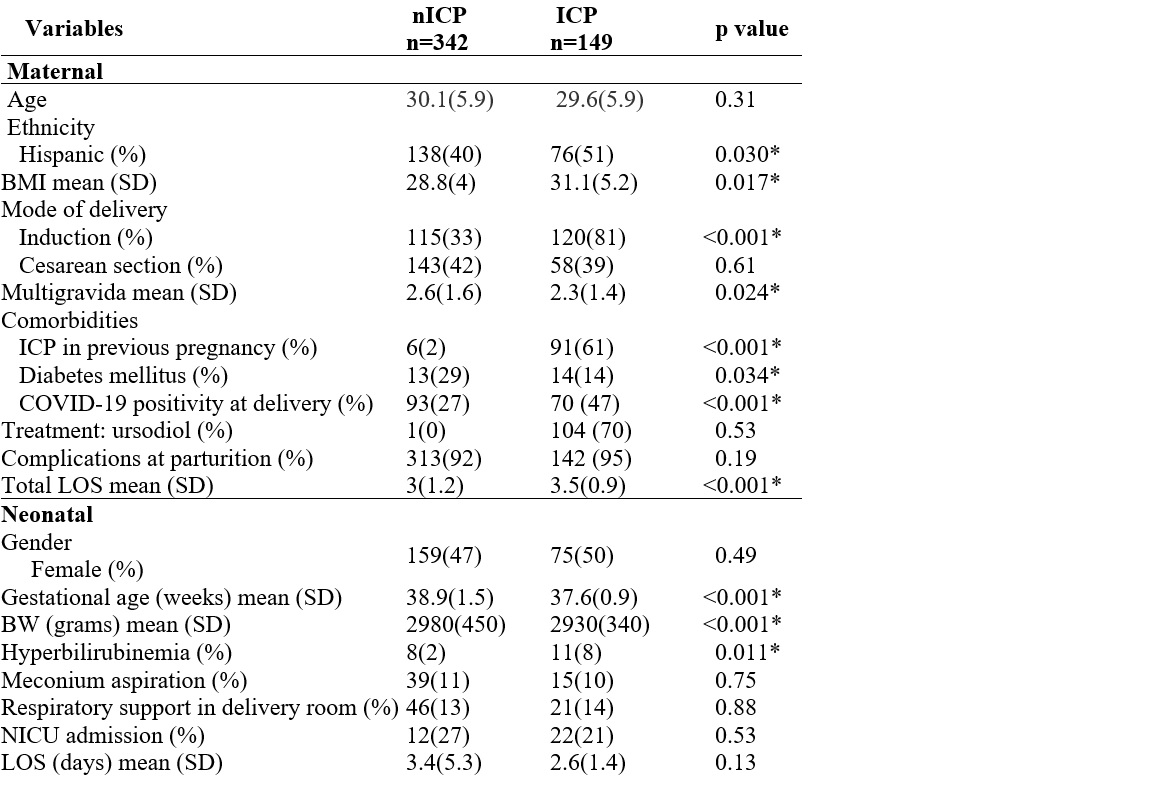
Design/Methods: A retrospective chart review of term neonates born to mothers with ICP and without ICP (nICP) at an urban community hospital between January 1, 2022 and December 31, 2022. Data extracted from maternal EHR included age, ethnicity, BMI, mode of delivery, parity, ICP in previous pregnancy, diabetes mellitus (gestational, non-gestational), COVID-19 positivity at delivery, alanine aminotransferase (ALT), aspartate aminotransferase (AST), bile acids, treatment for ICP, complication at parturition and length of stay (LOS). Data extracted from neonate EHR included gender, gestational age (GA), birth weight (BW), hyperbilirubinemia, meconium aspiration (MAS), need for respiratory support in the delivery room, NICU admission and LOS. ICP group and nICP group were compared for the mother and the neonate. Data were analyzed using Pearson correlation coefficient, p< 0.05 considered significant.
Results: Of the 491 charts reviewed, 149 (30%) were mothers with ICP (cases) and 342 (controls) were without ICP. Mothers with ICP were Hispanic in greater proportion (51%), p=0.03, had higher BMI and were delivered earlier by induction, p< 0.001, table 1. In addition, most mothers with ICP were multipara, had ICP in previous pregnancy, COVID-19 positivity at the time of delivery and longer LOS, table 1. Liver enzymes were elevated including alanine aminotransferase (ALT) in 36%, aspartate aminotransferase (AST) in 51% and bile acids in 28%.
Neonates born to mothers with ICP had lower GA, lower BW and hyperbilirubinemia at birth hospitalization, table 1. There was no difference in other comorbidities including MAS, need for respiratory support at delivery, NICU admission and LOS between the groups.
Conclusion(s): In our urban community hospital, maternal ICP was significantly associated with earlier delivery by induction, ICP in previous pregnancy, COVID-19 positivity at delivery and longer maternal LOS. Infants with maternal ICP had significantly higher rate of hyperbilirubinemia at birth hospitalization.