Emergency Medicine
Session: Emergency Medicine 2: Operations
381 - Evaluating Differences in Pediatric Emergency Department Length of Stay by Language and Interpreter Type
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 381
Publication Number: 381.514
Publication Number: 381.514

Erin M. Hannon, MD
Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Use of interpreter services in the pediatric Emergency Department (ED) has been associated with reduced ED length of stay (LOS) for patients with limited English proficiency (LEP). While federal mandates require interpreter use, institutions use various interpreter types, including in-person, video and phone interpreters. Studies have shown higher rates of satisfaction among providers and families working with in-person interpreters, but few studies have investigated differences in clinical outcomes related to type of interpreter used.
Objective: To investigate differences in ED LOS by language and interpreter type.
Design/Methods: We conducted a retrospective analysis of patients seen in the pediatric ED of an urban academic hospital between 5/1 - 6/15/2022. A prior quality improvement initiative to improve documentation of interpreter use in the ED led to documentation rates > 90%. Patients were excluded if they had a preferred language other than English or Spanish (based on patient volume and in-person interpreter availability), or spoke Spanish but did not use an interpreter. Linear mixed effects models (by patient) were used to compare ED LOS by patient preferred language and interpreter type; models were adjusted for race and ethnicity, age, sex, triage severity, time of ED arrival, and primary insurance.
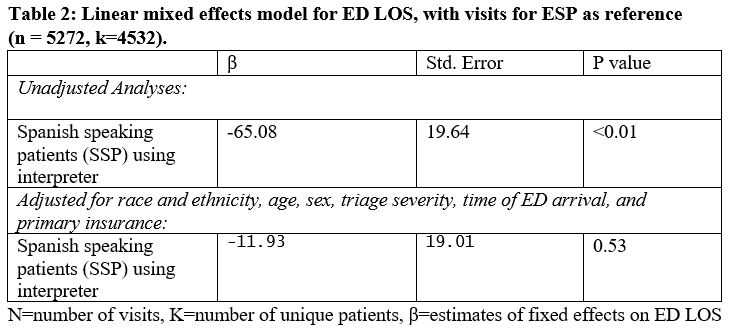
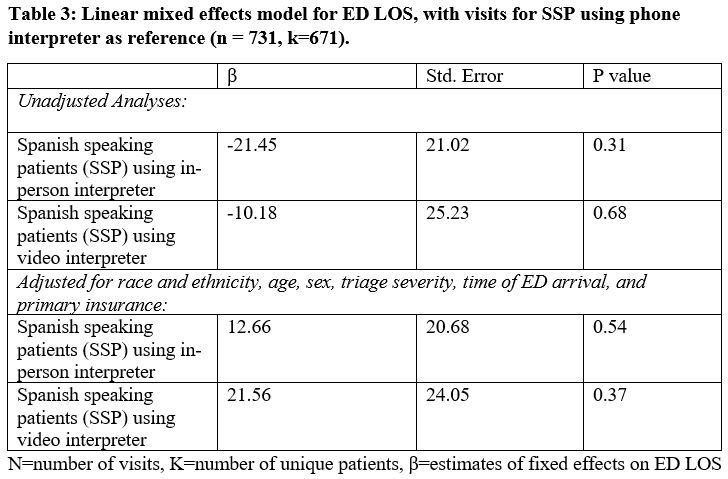
Results: There were 5272 total ED visits, which included 4541 English speaking patients (ESP) and 731 Spanish speaking patients who used interpreters (SSP). For visits with SSP, 401 used phone, 204 used in-person, and 126 used video interpreters (Table 1). Unadjusted mean ED LOS was longer for ESP than SSP (316 vs. 254 minutes, p = < 0.01). When adjusted for covariates, there were no longer significant differences (p = 0.53, Table 2). For SSP, interpreter type was not associated with ED LOS in either unadjusted or adjusted analyses (Table 3).
Conclusion(s): ED LOS was longer for ESP than SSP in unadjusted but not adjusted analyses. For SSP, there were no differences in ED LOS based on interpreter type. Future studies should examine reasons for differences in ED LOS by language, which may include differences in provider communication and/or the shared decision-making process.
.jpg)