Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
195 - Predicting pulmonary hemorrhage in extremely low birth weight (ELBW) infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 195
Publication Number: 195.2901
Publication Number: 195.2901
- NL
Natasha Lalos, MD (she/her/hers)
Fellow Physician
Washington University in St. Louis School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Pulmonary hemorrhage in extremely low birth weight (ELBW) infants is a catastrophic event with significant mortality, upwards of 50%. However, the clinical ability to predict pulmonary hemorrhage is poor and there are no tools to aid in detection. Recent advances in machine learning may allow identification of subclinical physiologic biomarkers to provide early warning.
Objective: To identify candidate physiologic biomarkers using heart rate (HR) and pulse oximetry (SpO2) predictive of pulmonary hemorrhage events in ELBW infants.
Design/Methods: Vital sign data from preterm infants with birth weight < 1000g were retrospectively accessed from two level IV NICUs. At both sites, vital sign data (including HR and SpO2) are archived for research with data sampled every two seconds throughout NICU hospitalization. Infants with pulmonary hemorrhage were identified; the timing of the event and relevant clinical data were recorded.
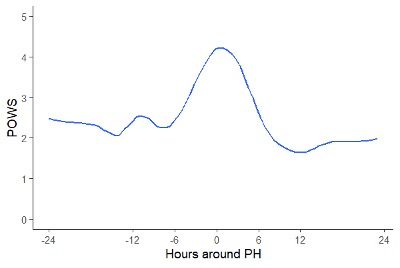
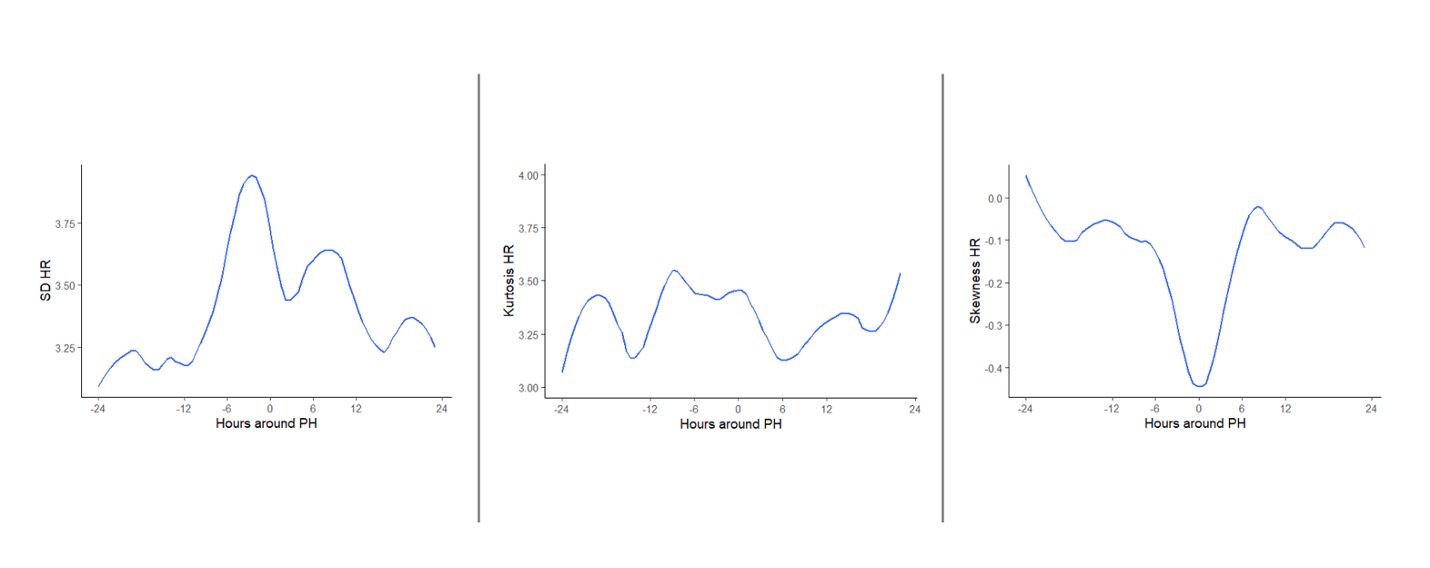
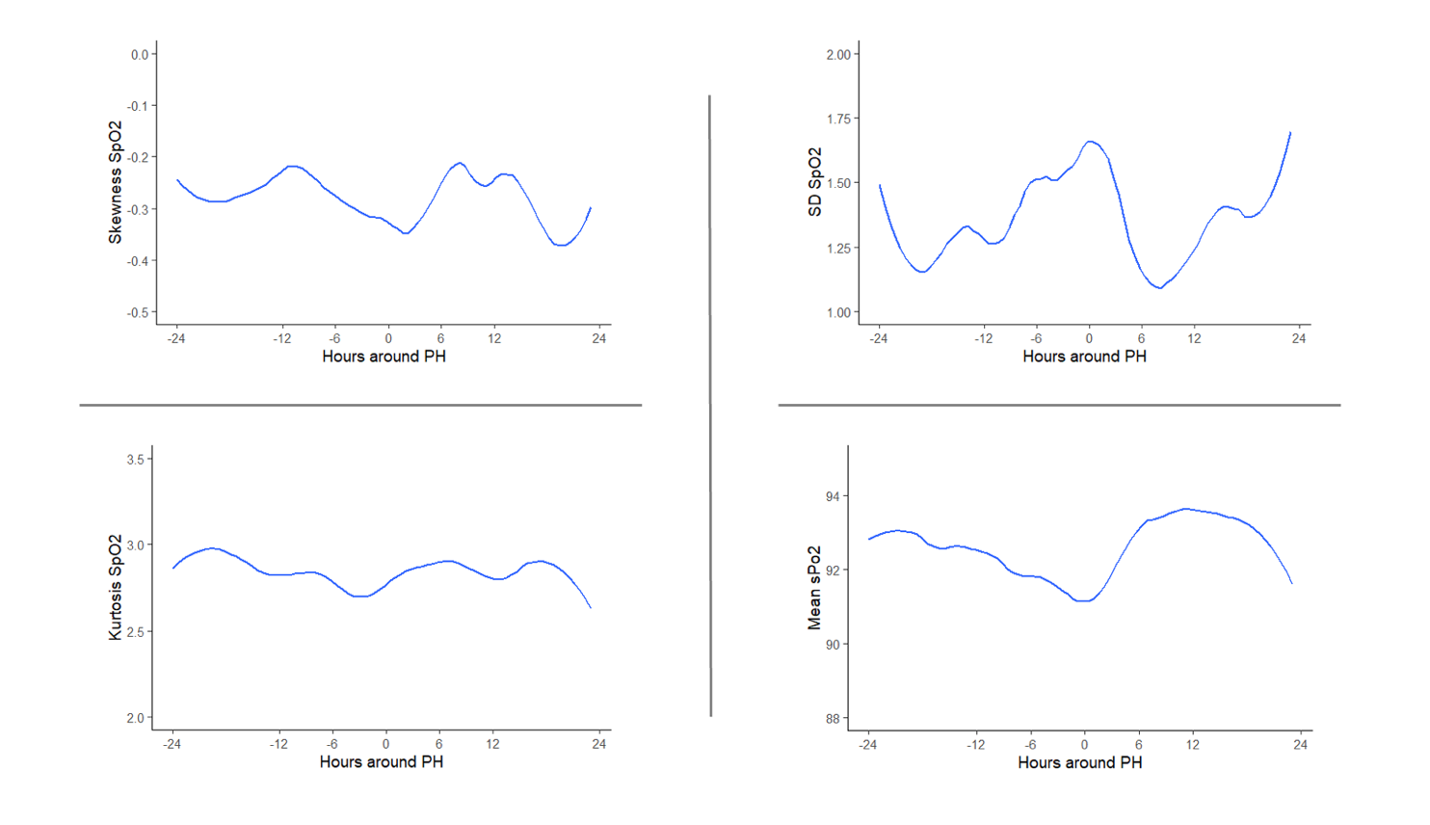
Using HR and SpO2 data from 24 hours before and after the hemorrhage event, we calculated hourly cardiorespiratory deterioration risk scores using a machine learning model developed to predict sepsis (called pulse ox warning system, POWS). POWS input features include the mean, standard deviation (SD), skewness, kurtosis and cross correlation of HR/SpO2. We evaluated POWS and individual input features by plotting each as a function of time to clinical diagnosis.
Results: We analyzed 29 infants with mean BW=695g, gestational age=25 weeks, 39% female, and 31% mortality. POWS demonstrated a two-fold rise, starting approximately 6 hours before the hemorrhage event (Figure 1). Examining individual POWS features, HR standard deviation increased, and HR skewness decreased in the hours before clinical diagnosis (Figure 2) and simultaneous increase in the standard deviation of SpO2 (Figure 3). Other features did not demonstrate a dynamic change near pulmonary hemorrhage diagnosis.
Conclusion(s): Using a machine learning model developed to predict cardiorespiratory deterioration due to sepsis, we identified signatures of pulmonary hemorrhage preceding the clinical diagnosis in data from two NICUs. Although additional validation is needed, this promising tool offers the potential for early diagnosis of pulmonary hemorrhage, which could allow for earlier interventions and improved outcomes.