Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 1
451 - Analysis of Neonatal PIVIs: Does Composition of Parenteral Nutrition Matter?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 451
Publication Number: 451.2993
Publication Number: 451.2993

Abigail O'Rourke, MD (she/her/hers)
Pediatric Resident
Cohen Children's Medical Center
New Hyde Park, New York, United States
Presenting Author(s)
Background: Neonates in NICU are at high risk for infiltration and extravasation of fluid from peripheral intravenous catheters (PIVI) because of the frequent cannulation of small and fragile vessels. The most common infusate in neonates is parenteral nutrition solution (PNS), followed by antibiotics. Previous reports have suggested that the intrinsic properties of infusates, such as pH, osmolality, and calcium content, determine the severity of PIVIs.
Objective: To determine the characteristics of infants and IV infusates that are associated with the development of severe neonatal PIVIs.
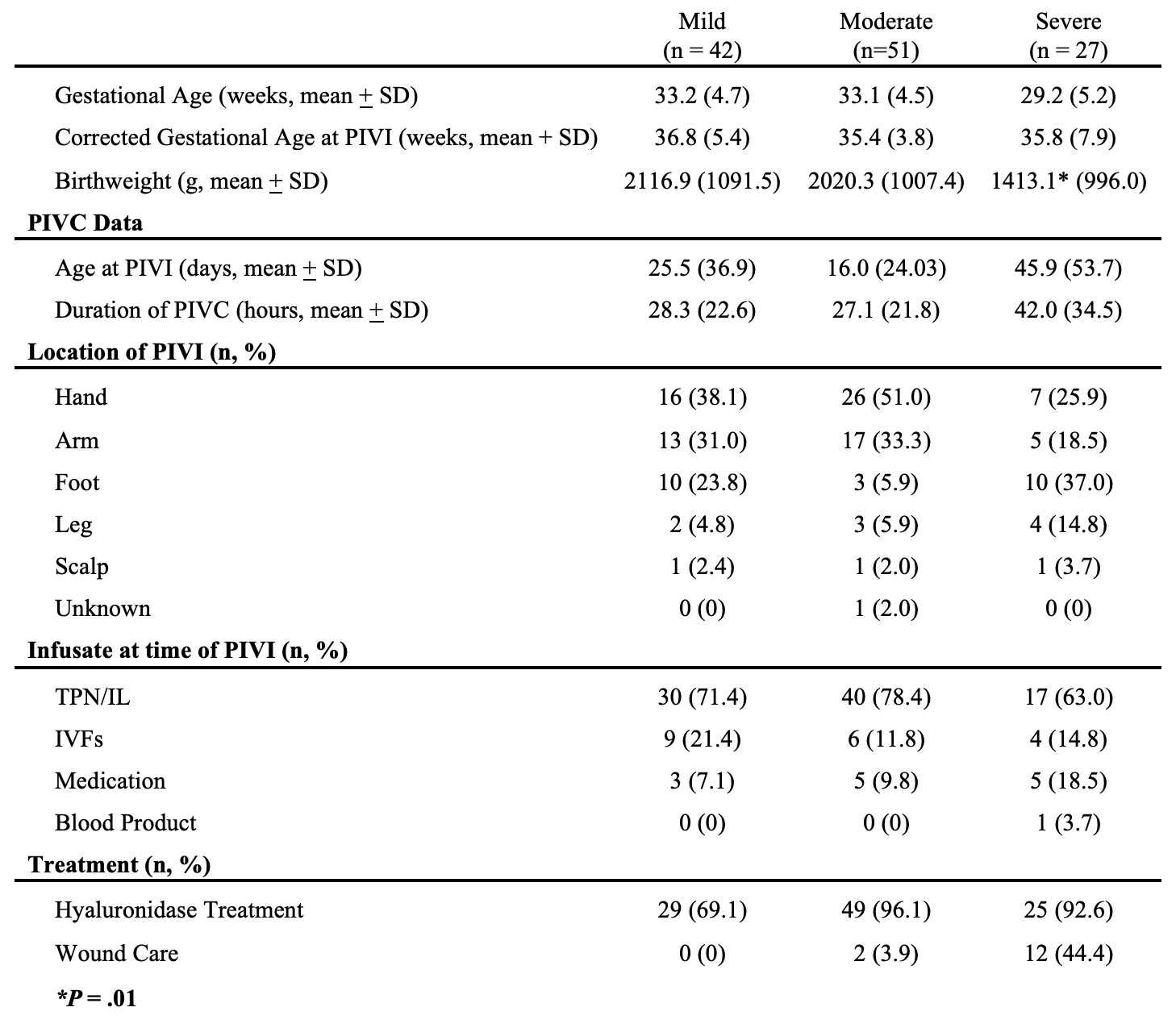
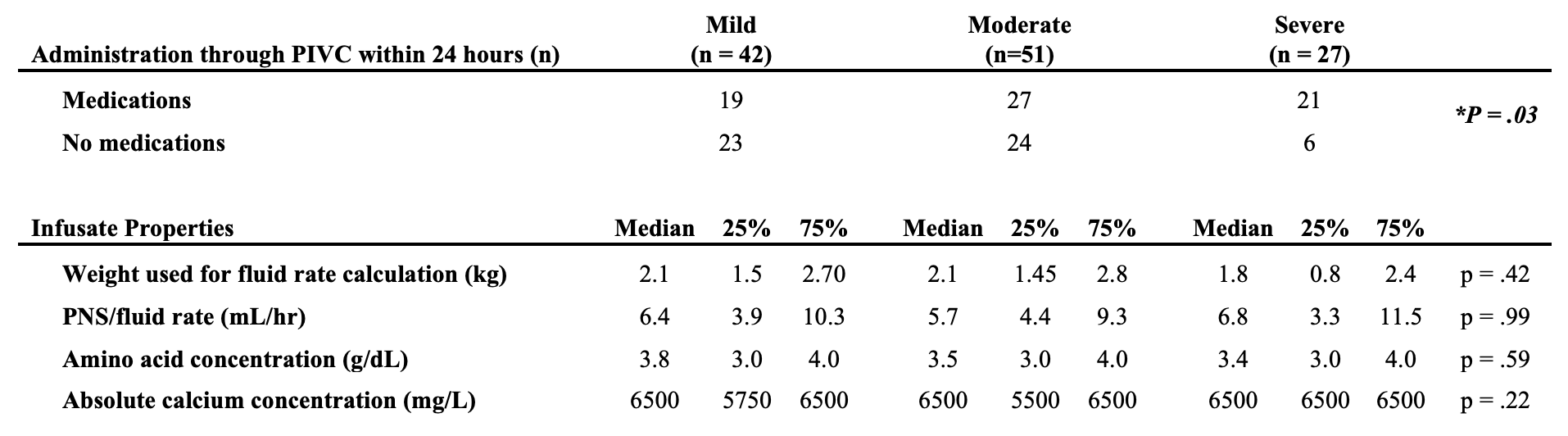
Design/Methods: We conducted a retrospective analysis of PIVIs in our level IV NICU from 2018-2022 (n=120). Each PIVI was evaluated by a wound-certified neonatologist and classified as mild, moderate, or severe using an internal scoring system based on Infusion Nurses Society (INS) staging and the Solutions for Patient Safety guide. Statistical comparisons between the severity groups included ANOVA and chi-square analyses.
Results: Infants with severe PIVIs had lower mean birthweight than those with mild or moderate PIVIs (1413.1 g vs 2116.9 g and 2020.3 g respectively, p = .01) (Table 1). Most PIVIs occurred during infusions of PNS and lipids, but the severity was not associated with the infusion rate or with the concentrations of amino acids (median 3.8 g/dL in the mild group and 3.4 g/dL in the severe group) or calcium (median 6500 mg/L in all groups). Of note, the infusion of intravenous medications within 24 hours of PIVI was most common in the severe PIVI group (P = .03) (Table 2). Most PIVIs, including mild, were treated with hyaluronidase. Wound care (dressing and/or topical product) was required for 4% of moderate and 44% of severe PIVIs, and none required surgical intervention.
Conclusion(s): Severe PIVIs in the NICU are most likely to occur in infants with low birthweight and within 24 hours of administration of IV medications. This is most likely because medications must be kept at acidic or basic pH for stability, and many have high osmolarity and/or intrinsic caustic properties. Thus, medications may induce chemical phlebitis and extravasation with inflammation. In contrast, PNS components, including amino acids and calcium, are not related to the severity of extravasation. Our findings suggest that increased surveillance of IV sites for preterm infants following medication administration may decrease the risk of severe PIVI. Conversely, withholding calcium or protein may introduce nutritional risks without decreasing the risk of clinically significant PIVIs.