Emergency Medicine
Session: Emergency Medicine 4: Infections
118 - Increasing HIV & Syphilis Testing for Adolescents in the ED
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 118
Publication Number: 118.1073
Publication Number: 118.1073
Taylor Jarvill, MD (she/her/hers)
Resident
Rady Children's Hospital San Diego
San Diego, California, United States
Presenting Author(s)
Background: Adolescents comprise a significant portion of new cases of sexually transmitted infections, but face many barriers to screening and treatment. Emergency departments (EDs) often act as safety nets for adolescents who would otherwise not access care in other health care settings, and can provide and arrange screening, treatment, and appropriate follow-up.
Objective: Our quality improvement (QI) initiative aimed to increase the proportion of ED patients >12 years undergoing peripheral IV (PIV) placement or phlebotomy who had HIV and syphilis screening tests done from 2.5 to 25% by May 31, 2023.
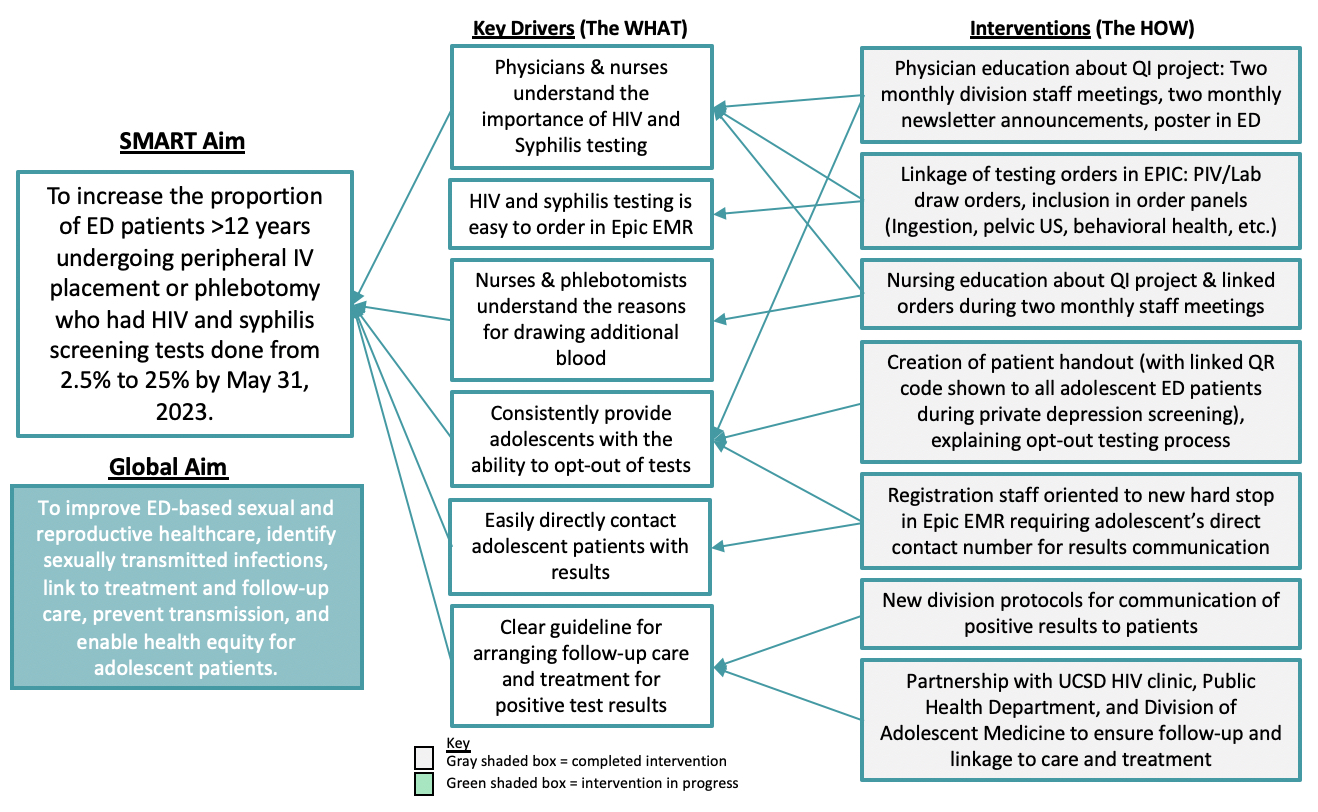
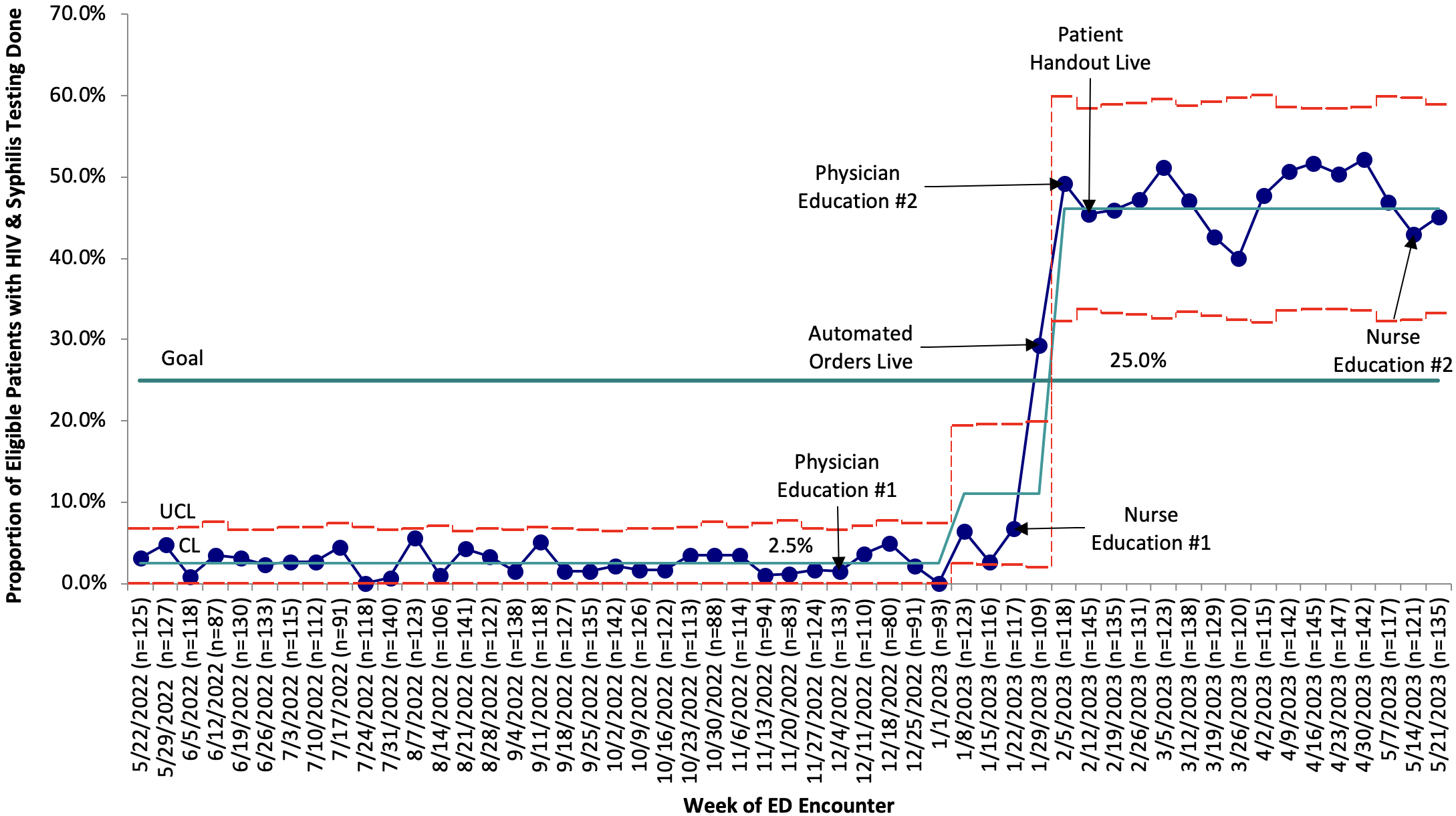
Design/Methods: Our multidisciplinary QI team was comprised of ED, infectious disease, and adolescent physicians; ED nursing; and hospital registration, lab, compliance, and informatics stakeholders. We constructed a key driver diagram, and identified multiple interventions for implementation (Figure 1). Our primary measure was the weekly proportion of adolescent ED visits requiring PIV or phlebotomy that had HIV and syphilis testing performed. Process measures included the proportion of the eligible population with gonorrhea and chlamydia testing done concurrently. Outcome measures included the proportion of HIV/syphilis tests that were positive and the proportion of patients with positive tests linked to care. Balancing measures included false positive results, and reported difficulties with disclosure and follow-up. Measures were analyzed using statistical process control to examine changes over time.
Results: From December 2022 to May 2023, the weekly proportion of eligible adolescents tested for HIV and syphilis increased from 2.5% to 46.1%, with the largest increase in testing occurring and sustained after testing orders were automatically linked to PIV and phlebotomy orders in the electronic medical record (Figure 2). 628/1096 (57.3%) of patients tested for syphilis and HIV were concurrently tested for gonorrhea and chlamydia. There were 7 false positive HIV tests and zero confirmed positive. Syphilis testing detected 2 confirmed cases of primary syphilis, 7 false positives, and 4 patients with preliminary positive results that were lost to follow-up.
Conclusion(s): Using QI methodology, we successfully increased the proportion of ED patients >12 years old screened for HIV and syphilis, with the greatest increase after order automation. Potential future directions include expansion of screening to include Hepatitis C and implementing a health care navigator to support follow-up testing and linkage to care.