Neonatology
Session: Neonatal Neurology 5: Clinical
536 - Factors associated with Periventricular Leukomalacia in very low birth weight infants: A multicenter study in the NEOCOSUR Network
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 536
Publication Number: 536.1172
Publication Number: 536.1172
- MC
Maria V. Castillo (she/her/hers)
pediatrician
Pontifica Universidad Católica de Chile
Santiago, Region Metropolitana, Chile
Presenting Author(s)
Background: The prevalence of Periventricular Leukomalacia (PVL) has remained stable in very-low-birth-weight (VLBW) infants at the NEOCOSUR Neonatal Network for 16 years.
Objective: Determine the factors associated with PVL in VLBW infants survivors at discharge. Additionally, determine the incidence and stratified by gestational age (GA).
Design/Methods: This is a multicenter, observational, retrospective cohort study with prospectively collected data, using the NEOCOSUR Neonatal Network database. All premature infants born in network centers between 2012-2021, survivors at discharge, with birth weight between 400 to 1500 grams at birth and 23 to 31+6 weeks GA, were included. Patients with major congenital malformations were excluded. A bivariate analysis was performed using Pearson's chi-square test to contrast the percentage of PVL for categorical variables and the t-student test to compare means for numerical variables. A multivariate logistic regression analysis was performed to explore the independent effect of each variable.
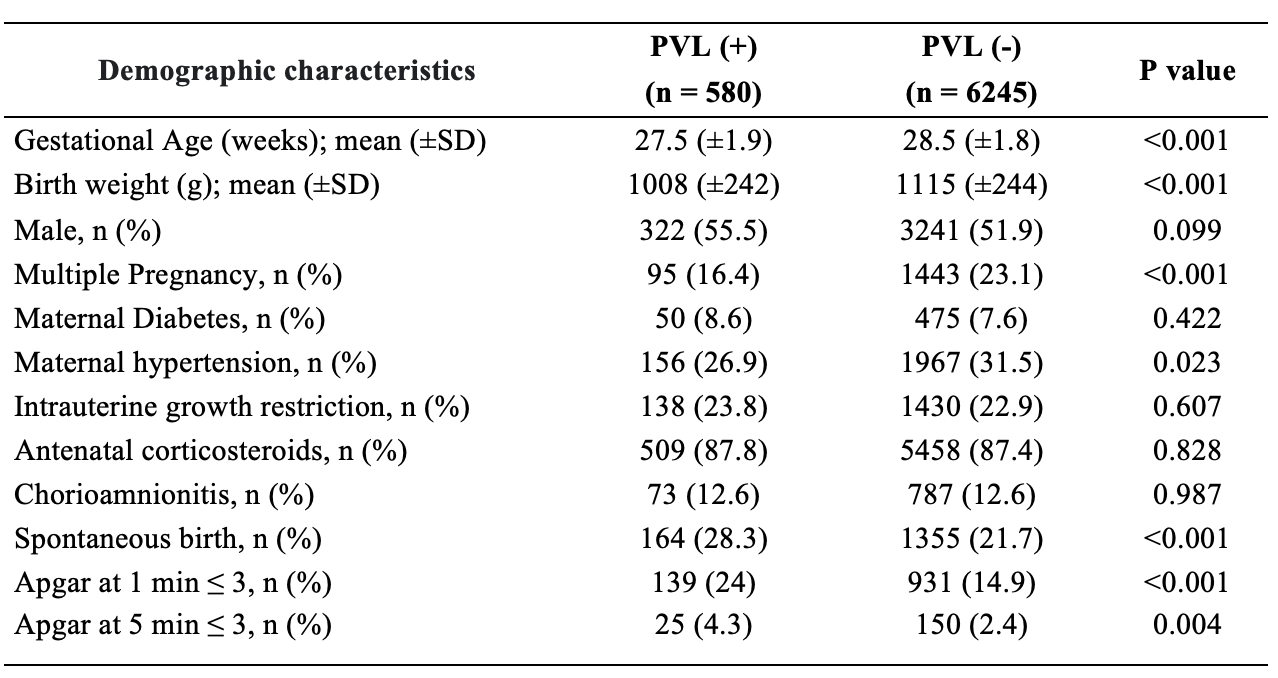
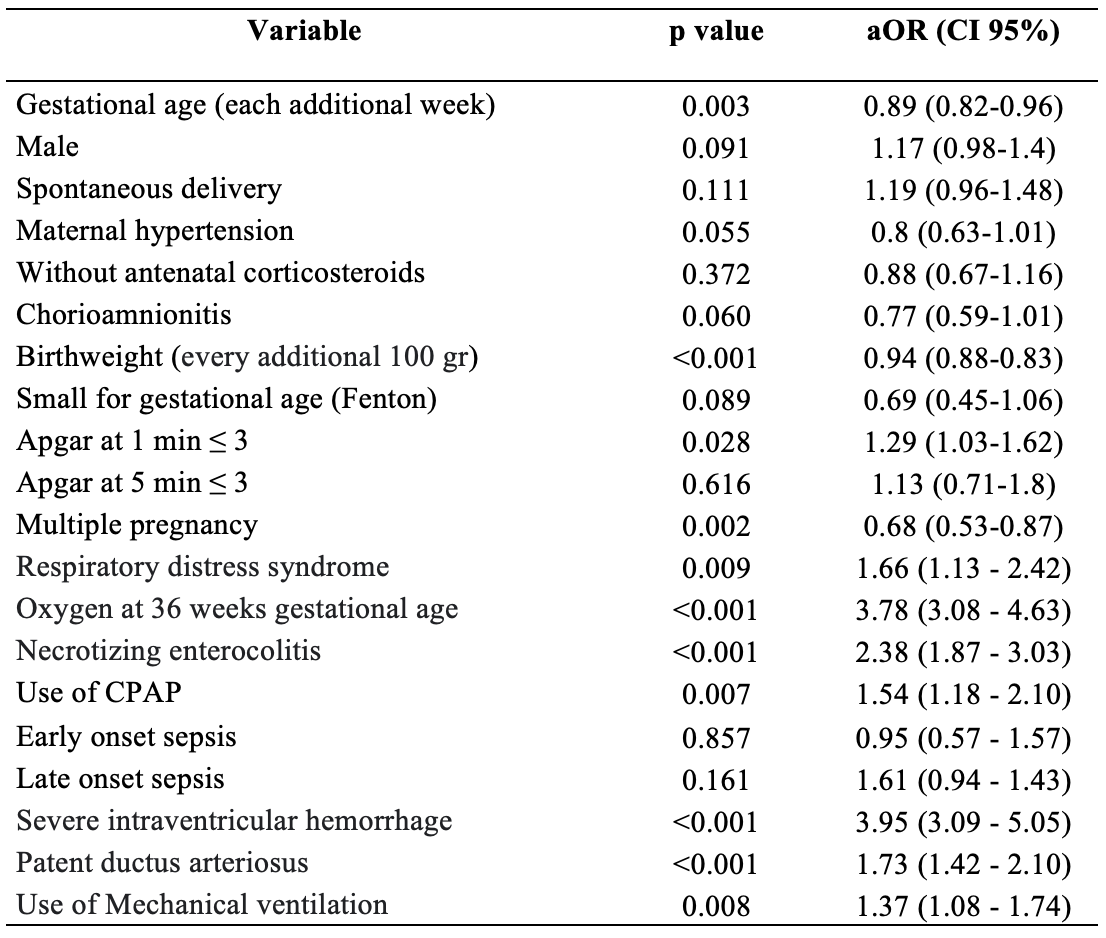
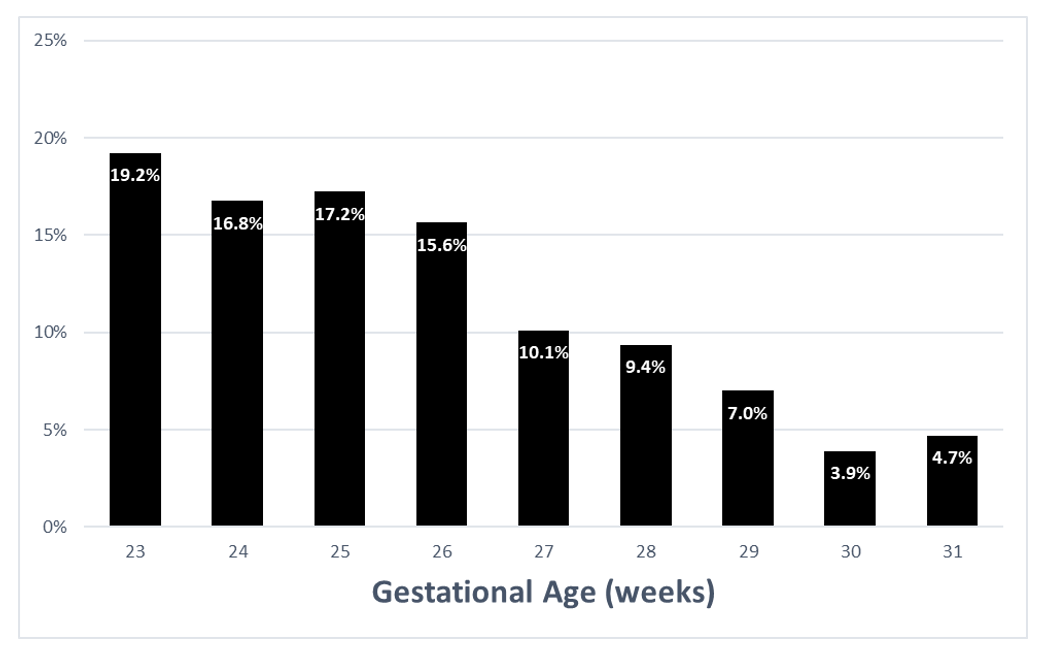
Results: A total of 6825 patients were analyzed. Demographic characteristics are shown in Table 1. Morbidities and therapies associated with an increased probability of PVL were bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), severe intraventricular hemorrhage (IVH), patent ductus arteriosus (PDA), respiratory distress syndrome (RDS), use of CPAP and mechanical ventilation (MV) (Table 2). The overall incidence of PVL was 8.5% in survivors at discharge, increasing at lower gestational age (Figure 1).
Conclusion(s): BPD, NEC, severe IVH, PDA, RDS, use of CPAP, and use of MV were associated with a higher probability of PVL. The overall incidence of PVL in survivors was 8.5%, increasing at lower gestational age.