Emergency Medicine
Session: Emergency Medicine 8: Mental Health
579 - Readiness of United States Emergency Departments for Pediatric Behavioral Health Care
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 579
Publication Number: 579.1707
Publication Number: 579.1707

Ashley A. Foster, MD (she/her/hers)
Assistant Professor, Emergency Medicine
University of California San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: In the United States, emergency department (ED) utilization by children with behavioral health (BH) conditions is increasing. However, ED readiness to care for this vulnerable population is currently unknown.
Objective: We aimed to assess changes in BH readiness across United States EDs from 2013 to 2021. We also sought to determine ED-level characteristics associated with having recommended behavioral health policies.
Design/Methods: A retrospective cross-sectional study of National Pediatric Readiness Project (NPRP) assessments of all United States EDs, administered from 1/2013-8/2013 and 5/2021-8/2021 was conducted. A comparison of the percentage of EDs with BH assessment items in 2013 and 2021 was performed using McNemar tests. To determine the ED characteristics associated with presence of recommended BH assessment items from 2021 data, multivariable models were generated. Results were reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI).
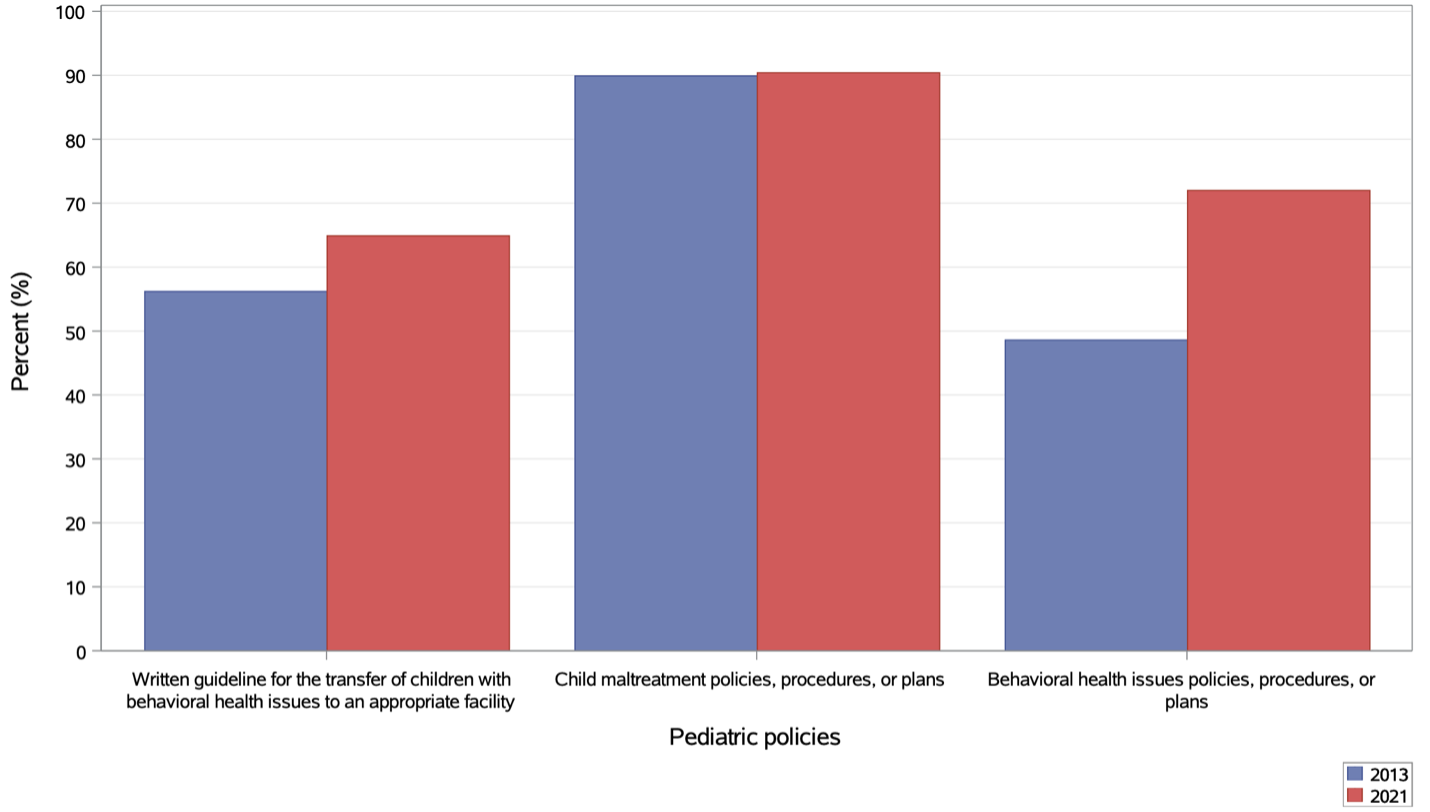
Results: Of 3,554 responding EDs in 2021, 62.9% were urban, 44.9% had trauma center designation, 55.8% were a general ED within a general hospital. Of EDs that completed both 2013 and 2021 NPRP assessments, the percentage that reported having BH policies increased from 48.6% to 72.0%; those with written transfer guidelines for children with BH issues increased from 56.2% to 64.9% (Figure 1). Adjusted odds of having BH policies in 2021 were lower in rural EDs (aOR 0.73, 95% CI 0.57, 0.92) and remote EDs (aOR 0.65, 95% CI 0.48, 0.88) compared to urban EDs (Figure 2). Odds of having transfer guidelines for children with BH issues were lower for suburban (aOR 0.71, 95% CI 0.54, 0.93), rural (aOR 0.61, 95% CI 0.48, 0.76), and remote EDs (aOR 0.54, 95% CI 0.40, 0.72) compared with urban EDs. Having trauma center designation was associated with lower odds of having behavioral health policies (aOR 0.80, 95% CI 0.67, 0.95), transfer guidelines (aOR 0.81, 95% CI 0.69, 0.95), and access to BH resources in the event of disaster (aOR 0.53, 95% CI 0.40, 0.71). Children’s hospitals and presence of both a nurse and physician pediatric emergency care coordinator (PECC) were associated with higher odds having behavioral health assessment policies.
Conclusion(s): Although ED readiness to care for children with BH conditions improved from 2013 to 2021, gaps remain, particularly among more rural EDs and at designated trauma centers. Having PECCs is a modifiable strategy for EDs to increase BH readiness.
.png)
