Neonatology
Session: Neonatology Pulmonology Clinical Science 3 - Oxidants/anti-oxidants, Lung Protection and It's Technical
596 - Feasibility of Applying Synchronized and Proportional Negative Pressure Ventilation in Preterm Infants with Respiratory Distress (NeoVest)
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 596
Publication Number: 596.1601
Publication Number: 596.1601

Jennifer BECK, PhD (she/her/hers)
Staff Scientist
Unity Health Toronto
Toronto, Ontario, Canada
Presenting Author(s)
Background: In preterm infants, applying negative pressure ventilation (NPV) may offer advantages to traditional methods of nasal continuous positive airway pressure (nCPAP). In a pre-clinical model, we recently described the “NeoVest”, a system consisting of a sealed abdominal interface and a ventilator that applies NPV in synchrony and in proportion to the diaphragm electrical activity (Edi). In animals with loaded breathing, the Neovest reduced Edi by 50% and demonstrated specific diaphragm unloading, without hemodynamic effects. The NeoVest system, and its interface, have yet to be evaluated in human infants.
Objective: Objective was to evaluate the feasibility of applying synchronized and proportional NPV with an abdominal interface in preterm infants.
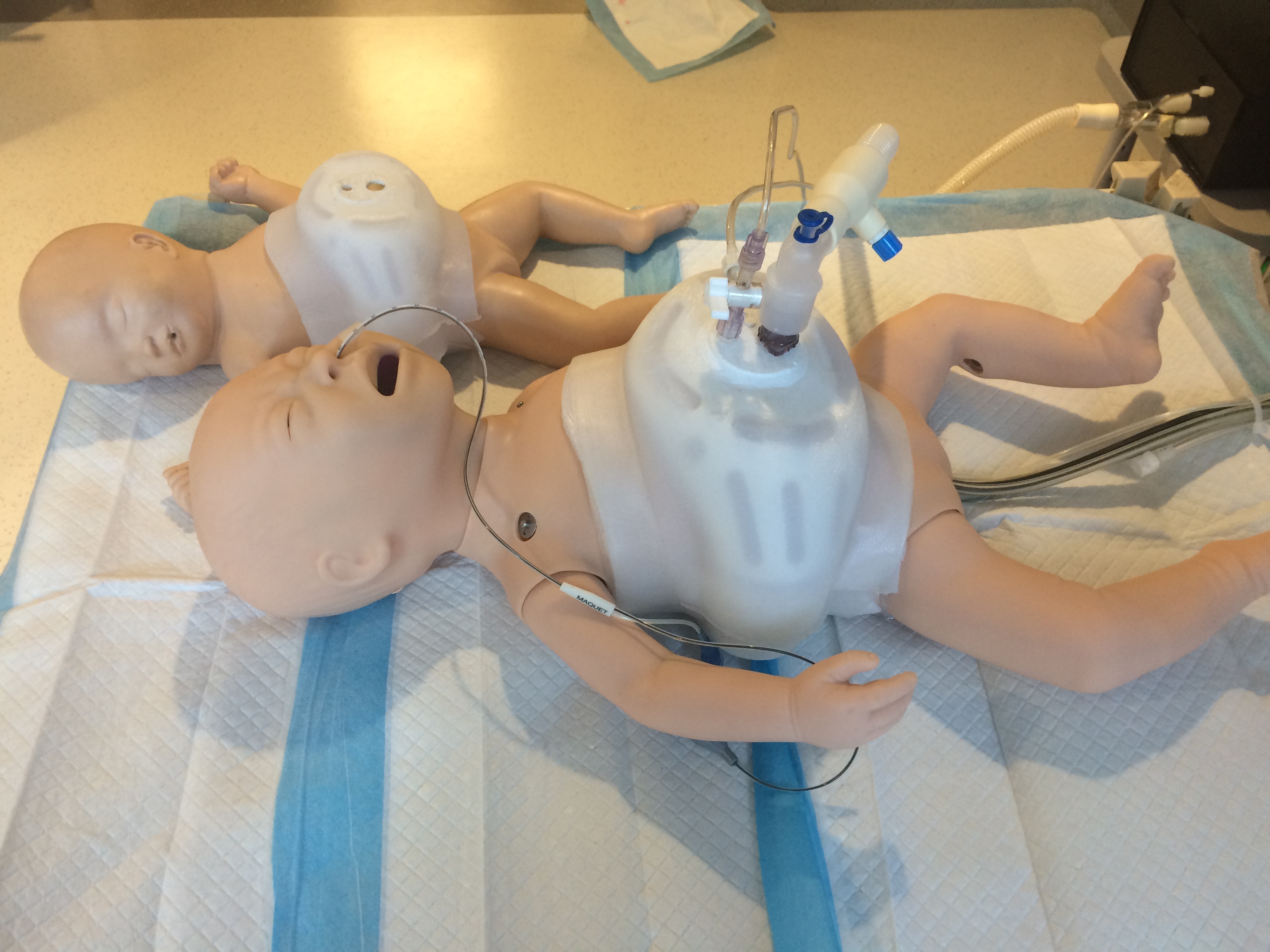
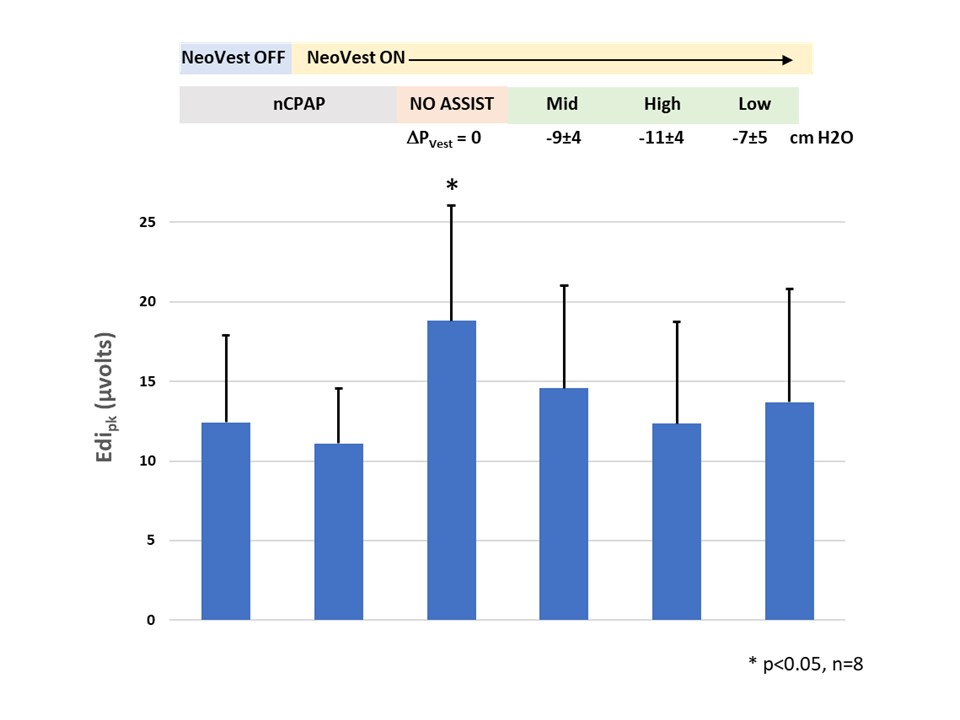
Design/Methods: This is a prospective feasibility trial. The inclusion criteria were admission to the Neonatal Intensive Care Unit with respiratory distress, birthweight>1.5kg, < 6 weeks old, FiO2 < 0.35, clinically stable with no recent apneas/ bradycardias, nCPAP < 8 cm H2O, >48 hrs old, or post-extubation. After parental consent, the feeding tube was exchanged for a 6F “Edi catheter” (used for feeding and measuring Edi), and sensors were placed for heart rate, oxygen saturation, transcutaneous CO2, and non-invasive blood pressure. Figure 1 shows the Neovest interface on a manikin. The five protocol steps were: nCPAP/NeoVest OFF (10 min), nCPAP/NeoVest ON (10 min), NO ASSIST (1 min), NeoVest mid (10 min), NeoVest high (5 min), NeoVest low (5 min) (Figure 2).
Results: Eight babies were included. The principal diagnoses were RDS and TTN. Mean weight was 2186±480g and age 10±8 days old. All babies tolerated the physical application of the vest. As shown in Figure 2, there was no significant difference in Edipk when the vest was placed (12.4±5.5 vs. 11.1±3.5 uV). During the period of no assist, Edipk was higher (18.8 ±7.3 uV) than nCPAP or NeoVest periods (p= 0.012), which were not significantly different from each other. Neural respiratory rate was the same for all periods tested. As per its design, the Neovest system delivered negative pressure in synchrony and in proportion to the Edi. . Negative pressures applied (PVEST) were -9±4, -11±4, and -7±5 cmH2O for the three NeoVest periods (Figure 2). All infants were clinically stable with no disruptions to vital signs.
Conclusion(s): Applying synchronized and proportional negative pressure with the NeoVest system is feasible and shows promise with regards to diaphragm unloading. Future studies are required to evaluate the NeoVest in sicker babies, for longer periods and compared to other methods of respiratory support.