Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
182 - Pulmonary Vascular Abnormalities in Patients with Bronchopulmonary Dysplasia using Magnetic Resonance Imaging
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 182
Publication Number: 182.3253
Publication Number: 182.3253

James A. Rowe, MD (he/him/his)
Neonatology Fellow
Cincinnati Children's Hospital Medical Center
Fort Wright, Kentucky, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is a life-long morbid condition that is increasing in prevalence despite advances in neonatal infant care. Severe BPD is often associated with pulmonary hypertension with vascular abnormality and vascular pruning that is thought to lead to long-term reduction of pulmonary function and earlier mortality. Therefore, a method to directly assess distal pulmonary vascular abnormalities in these patients is needed to assess disease severity and to predict long-term outcomes.
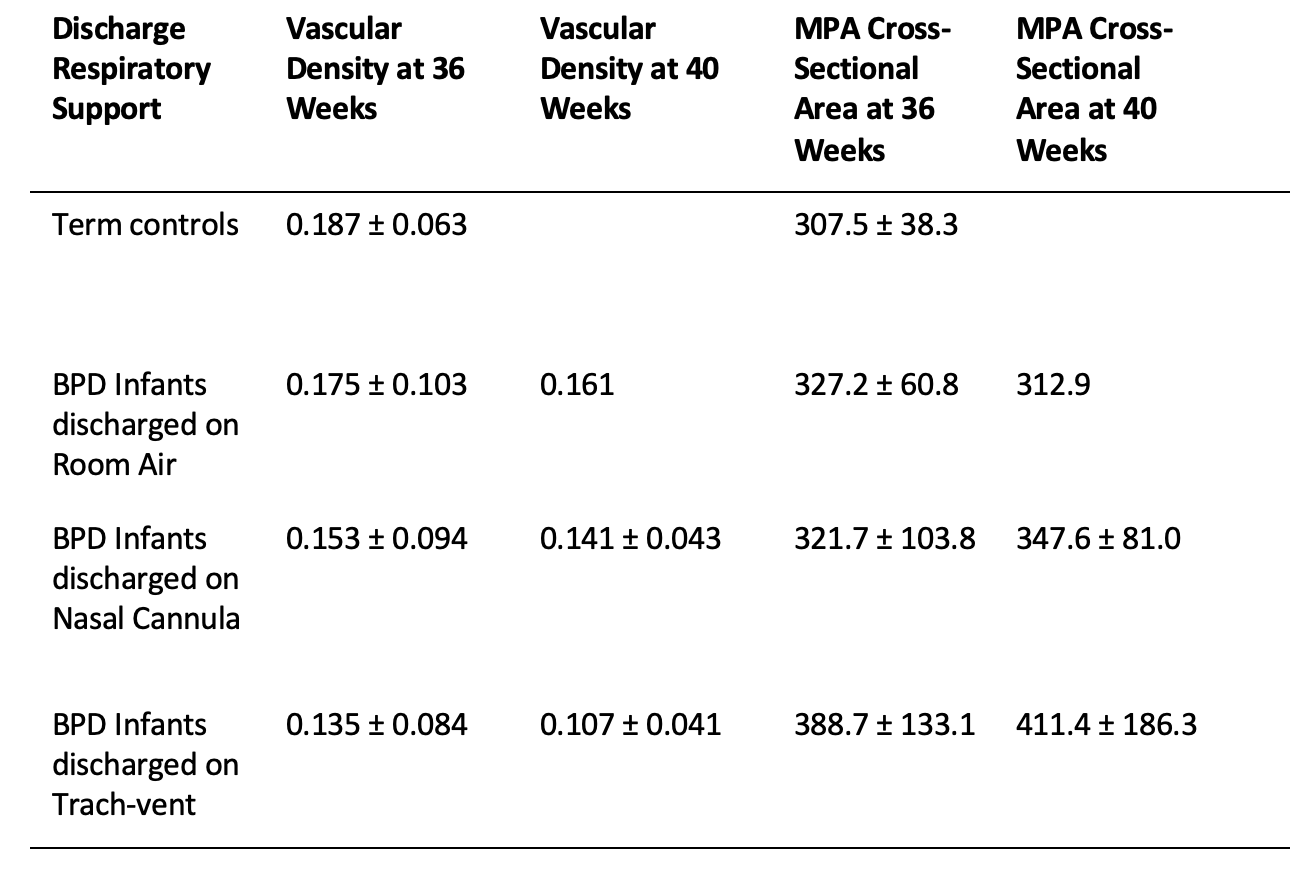
Objective: We hypothesize that vascular density and the coronal-plane cross-sectional area of the main pulmonary artery (mm2) will be associated with BPD severity and respiratory support at discharge.
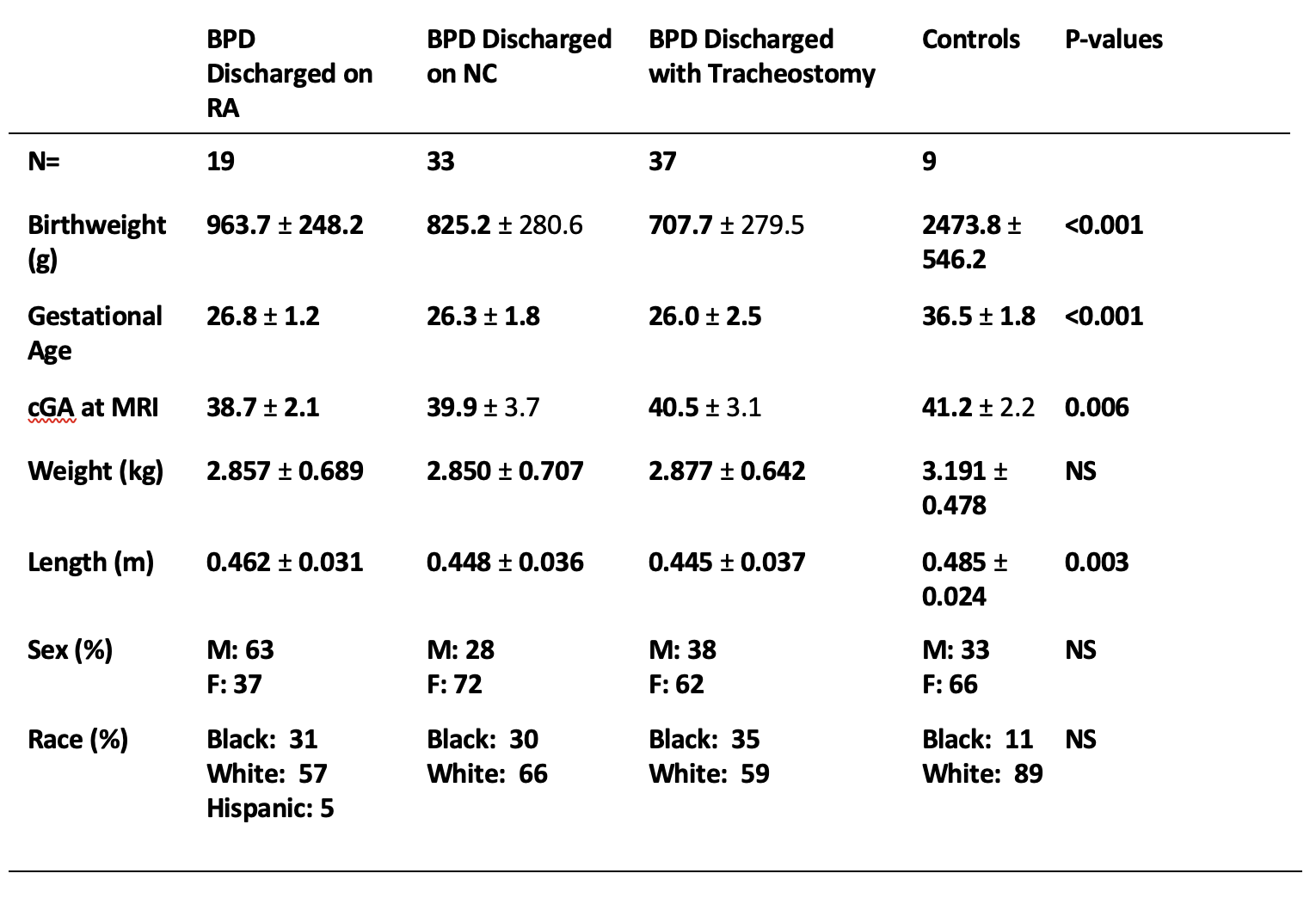
Design/Methods: Inclusion criteria are infants born less than 28 weeks with a diagnosis of BPD. Exclusion criteria are congenital heart disease, suspected neurologic disorder, evidence of infection at the time of scan, and scans with significant motion artifact. MRI scans occurred at ~36-weeks gestation, term, and post-term. Cross-sectional area was calculated using AnalyzePro Segmentation Software and was controlled for by body surface area. Vascular density was calculated as total lung vascular volume divided by total lung parenchymal volume.
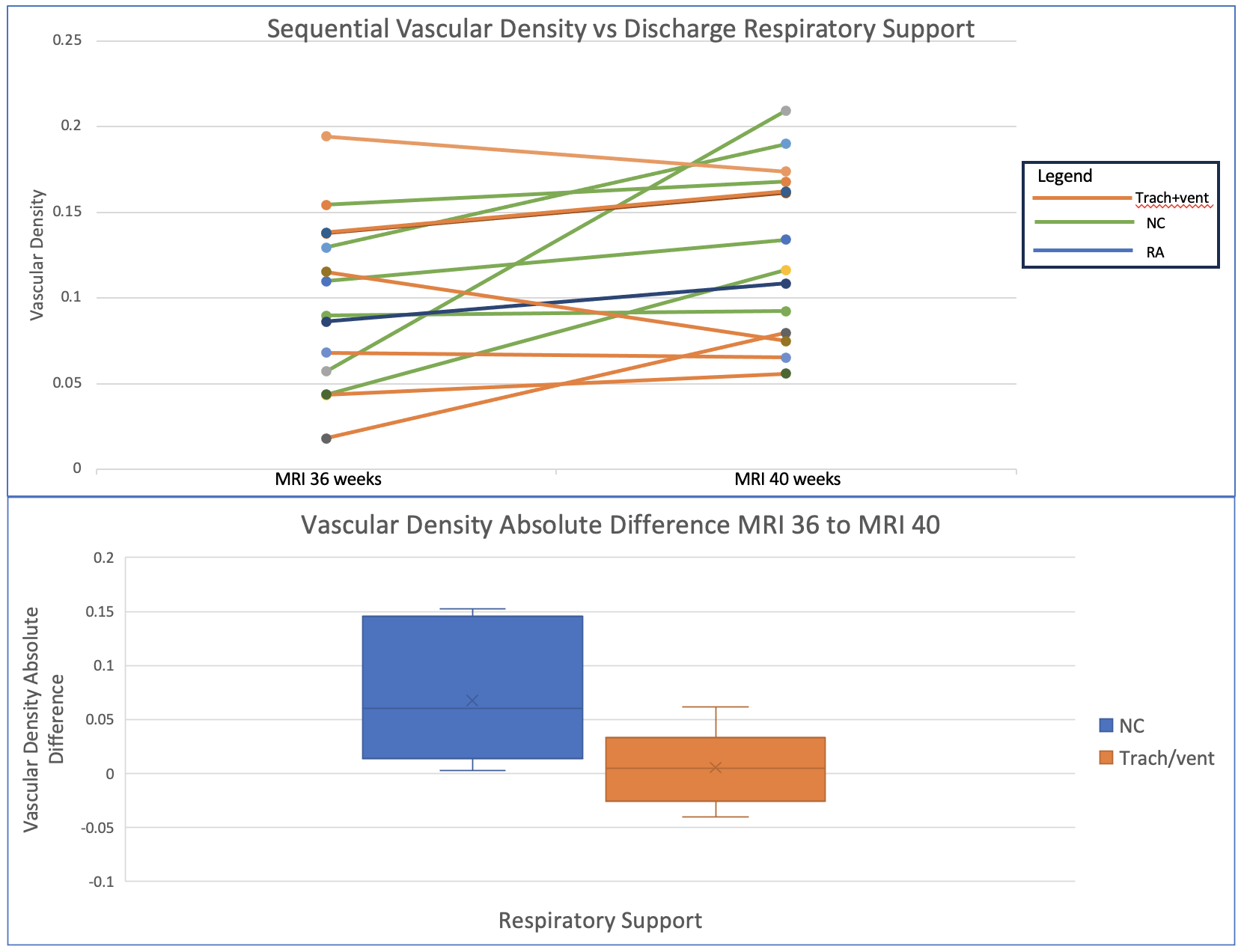
Results: In this retrospective study, 96 infants received MRI scans from 2014-2022. Infants were divided into controls without lung disease, infants with BPD discharged on room air, infants with BPD discharged on nasal cannula, and infants with BPD requiring tracheostomy. Infants requiring tracheostomy had lower vascular density than infants with BPD discharged on room air and nasal cannula but this did not reach statistical significance (p=0.09) (Table 2). Infants requiring tracheostomy had a trend towards upstream dilation of their main pulmonary artery (p=0.09) (Table 2). Twelve infants requiring mechanical ventilation at 36-weeks gestation had a follow up MRI at term gestation. Among this smaller cohort, those that successfully extubated had a higher rate of change of vascular density compared to those not able to be extubated (p=0.05) (Figure 1).
Conclusion(s): Infants requiring more respiratory support had decreased vascular density and concordant upstream dilation of the MPA as early as 36 weeks corrected. Infants followed with sequential MRI showed that those who were able to be weaned from positive pressure ventilation had a significant increase of their vascular density. Taken together, these results suggest that both absolute vascular density and changes in vascular density over time correlate with long term outcomes in infants with BPD.