Emergency Medicine
Session: Emergency Medicine 3: Serious Bacterial Infections
87 - Discriminating bacteremia from contaminants among children with a preliminary positive blood culture in the emergency department
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 87
Publication Number: 87.1592
Publication Number: 87.1592

Jocelyn Gravel, MD, MSc (he/him/his)
Attending
CHU Sainte-Justine
Montreal, Quebec, Canada
Presenting Author(s)
Background: Children with preliminary positive blood cultures in the emergency department (ED) often prompt urgent actions due to the risk of bacteremia. Distinguishing true bacteremia from contaminated cultures is crucial to safely prevent unnecessary, potentially harmful interventions.
Objective: This study aimed to assess a peer institution algorithm for discriminating bacteremia from contaminants in discharged ED patients, and to identify variables associated with bacteremia in children with positive blood cultures.
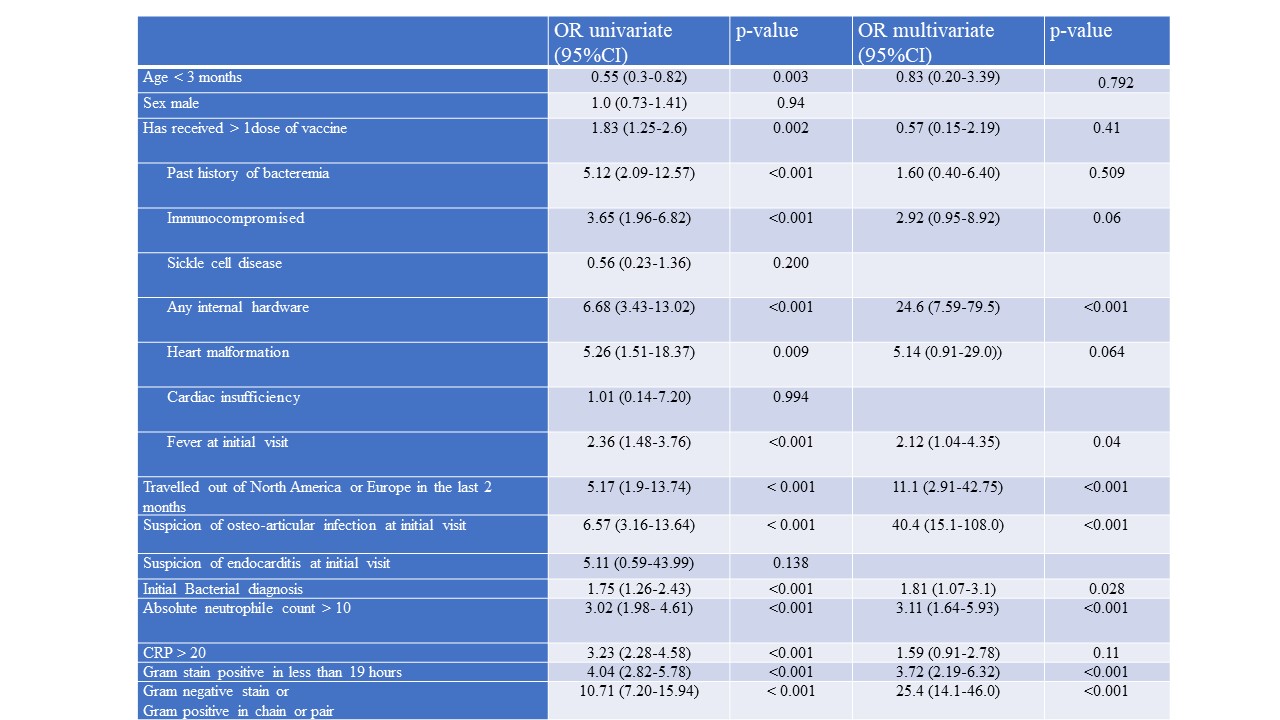
Design/Methods: This was a retrospective study of all children with positive blood cultures from a tertiary care, pediatric ED between 2018 and 2022. The primary outcome was true bacteremia as defined using a two-step standardized approach based on the bacteria involved and the clinical outcome assessed by two reviewers for each case. The independent variables assessed were demographic data (age and sex), presence of underlying disease, initial blood tests (CBC, CRP), Gram stain, time for positivity (in hours), presence of alternative diagnosis, fever at phone follow-up. The association between independent variables and outcome was measured using logistic regression. It was estimated that a sample of 500 participants would yield at least 200 true bacteremias and allow the evaluation of 20 risk factors.
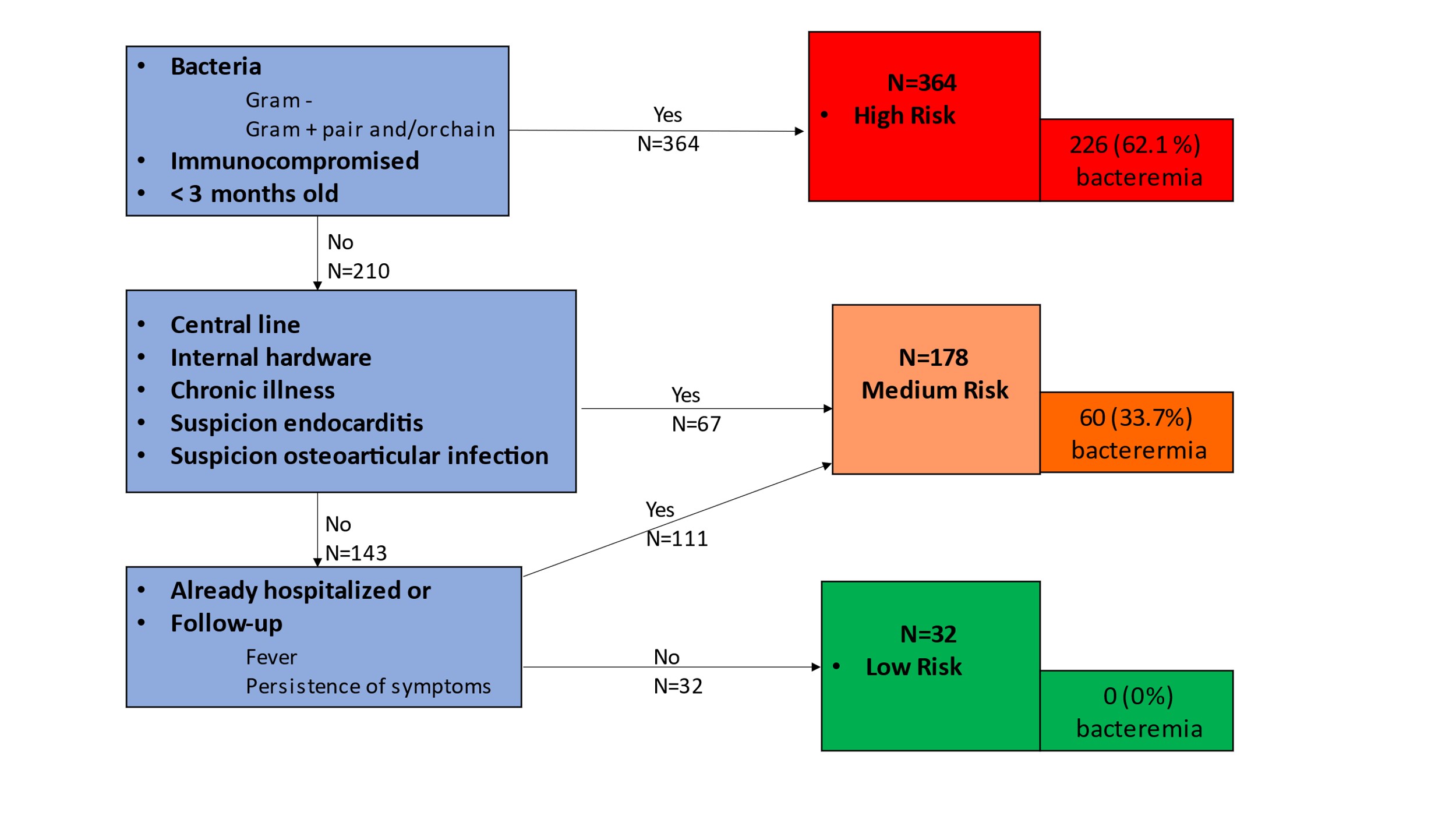
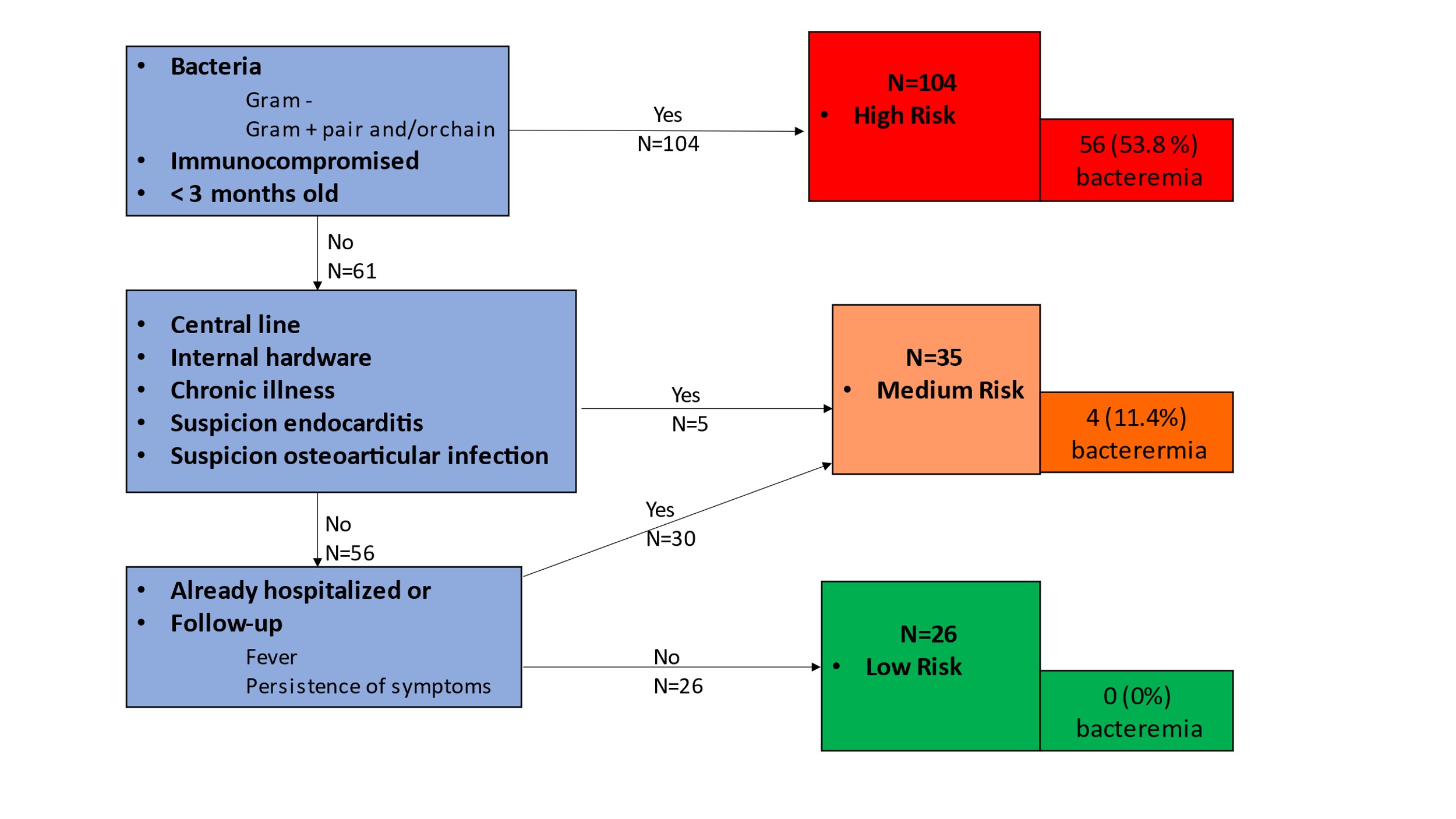
Results: 574 participants; 286 (49.8%) with bacteremia and 288 (50.2%) with contaminants were included. Utilizing the algorithm, 364 children (63%) were classified as high risk of true bacteremia, 178 (31%) as medium risk, and 32 (6%) as low risk. Corresponding bacteremia probabilities were 62%, 34%, and 0%, yielding 100% sensitivity (95% CI: 94-100%) and 11% specificity (95% CI:7.7-15%). A sub-analysis restricted to the 165 patients who were initially discharged classified 104 (63.0%) children at high risk, 35 (32.1%) at medium risk and 26 (15.7%) at low risk with proportions of bacteremia of 53.8%, 11.4% and 0 % respectively. The most significant predictors of bacteremia included suspicion of osteoarticular infection (OR: 40.4), presence of internal hardware (OR: 24.6), presence of Gram negative bacteria or Gram positive cocci in chains/pairs (OR: 25.4), and positivity within 19 hours (OR: 3.72).
Conclusion(s): While half of the positive blood cultures in our pediatric ED are contaminants, multiple risk factors of true bacteremia were identified. A peer institution algorithm is 100% sensitive to detect discharged patients with bacteremia, it demonstrated low specificity in our population. Multiple improvements opportunities are identified.