Neonatology
Session: Neonatal Neurology 3: Clinical
33 - Real-time EEG Brain State of Newborn Predicts Neonatal Encephalopathy Severity and Neurodevelopmental Outcome
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 33
Publication Number: 33.171
Publication Number: 33.171

Srinivas Kota, n/a
Assistant Professor
UT Southwestern Medical Center
Dallas, Texas, United States
Presenting Author(s)
Background: Hypoxic ischemic encephalopathy (HIE) is one of the leading causes of mortality and morbidity in newborns. While therapeutic hypothermia (TH) is standard clinical care for moderate and severe grades in developed countries, the management of mild HIE is controversial due to difficult clinical classification and progression of encephalopathy grade. We hypothesize that Brain State of Newborn (BSN) can accurately and quickly differentiate newborns with HIE based on its severity on the first day of life, which could help identify those who would benefit from neuroprotective therapies.
Objective: To assess a BSN derived from electroencephalogram (EEG) to distinguish newborns with HIE and predict neurodevelopmental outcomes at two years of age.
Design/Methods: Prospective cohort study of newborns at 36 weeks’ gestation or later with HIE at birth. BSN was calculated using the first day of EEG recording central and parietal inter and intra hemispheric bipolar EEG. The mean BSN value was calculated from artifact-free segments within a three-hour segment for statistical analysis. The Total Sanart Score (TSS) was calculated based on a modified Sarnat exam. The primary outcome at two year of age was a diagnosis of death or disability using Bayley Scales of Infant Development III cognitive, language or motor scores. To evaluate the prediction ability of BSN on encephalopathy and neurodevelopmental outcomes, we conducted the receiver operating characteristic (ROC) curve, with the area under the ROC curve (AUC). Results were reported as odds ratios (ORs) with 95% confidence intervals in logistic regression models.
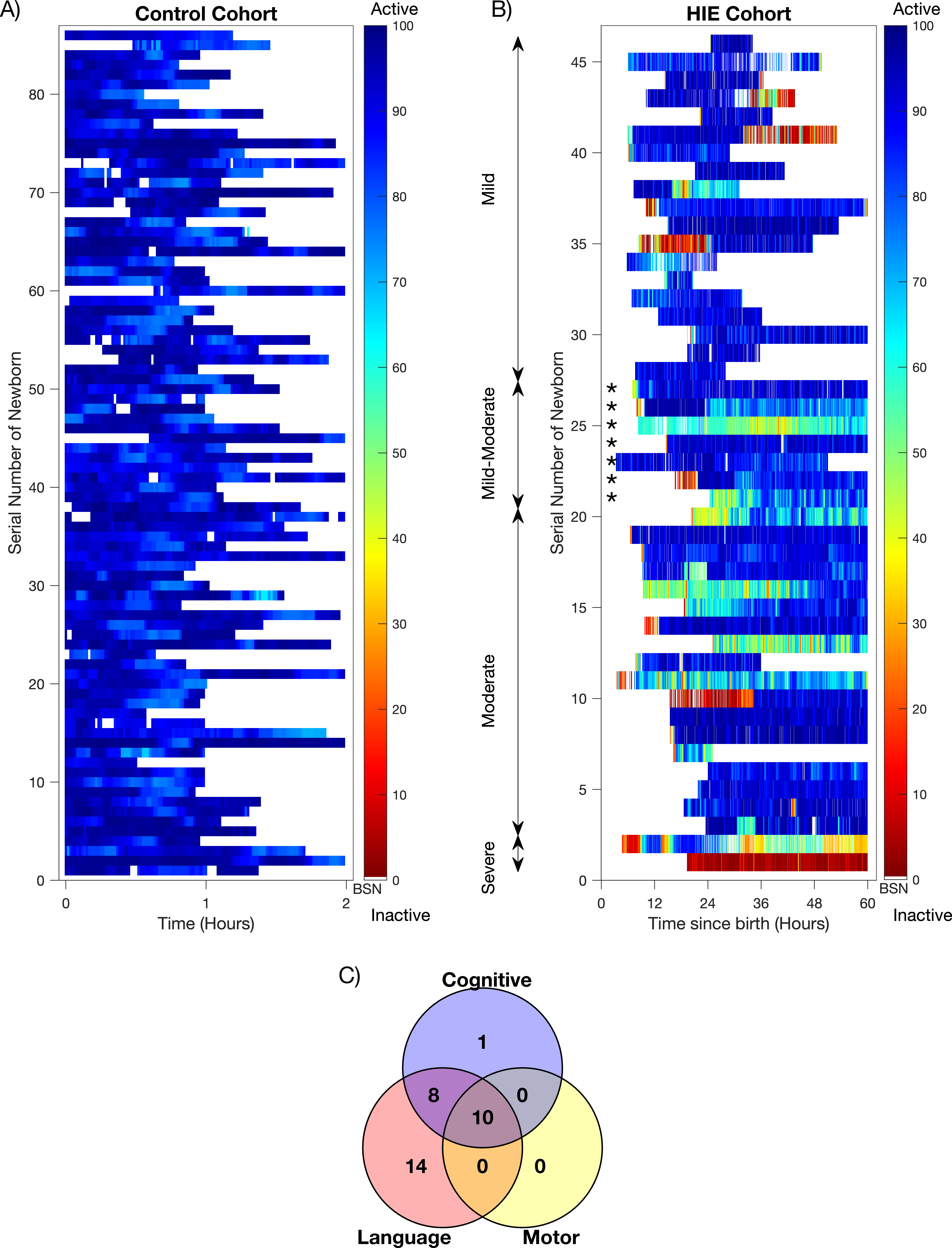
Results: Study enrolled 46 newborns with HIE and 86 controls. Figures 1A, B show clear visual distinction of BSN values between cohorts. Figure 1C shows some infants with more than one abnormality at two years of age.
BSN value of 85 distinguished normal from HIE (AUC 0.885, 95%CI: 0.746-1) and differentiated between normal and abnormal neurodevelopmental outcomes (AUC 0.940, 95%CI 0.850-1.0). In addition, infants with higher BSN values had lower odds of HIE (OR, 0.669; 95% CI, 0.533 - 0.839; p < 0.001) and abnormal neurodevelopmental outcome (OR, 0.826; 95% CI, 0.715 -0.953; p < 0.001) as early as 6 hours after birth.
Conclusion(s): BSN is a sensitive real-time marker for monitoring encephalopathy progression and predicting neurodevelopmental impairment, especially when the neurological exam inaccurate within the first six hours after birth, particularly for identifying dynamic mild encephalopathy cases that would benefit from neuroprotection therapies.