Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 6
47 - Advocacy in Foster Care: Improving Standard of Care for Children Entering Foster Care
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 47
Publication Number: 47.3085
Publication Number: 47.3085
- KG
Kathryn Guymon, DO (she/her/hers)
Assistant Professor/General Pediatrician
University of Missouri-Columbia School of Medicine
Ashland, Missouri, United States
Presenting Author(s)
Background: More than 700,000 children in the U.S. have spent time in foster care in the preceding 12 months. Children entering foster care are less likely to have had routine healthcare and little information is given to foster parents.
Objective: To establish standardized healthcare visits for children entering foster care seen at MU Healthcare based on AAP recommendations.
Design/Methods: Retrospective chart review was performed from 2018-2022 to obtain baseline care practices for children presenting to the emergency department, urgent care or pediatric clinics for the initial healthcare visit upon entering foster care. Implemented interventions included a) creation of electronic medical record (EMR) auto texts with standardized HPI, physical exam, and plan, b) educational didactics provided to emergency medicine and pediatric providers on AAP recommendations for the initial visit, and c) foster parent resource handout created and integrated into the EMR with information regarding medical visits and local resources. Pre- and post-intervention surveys were conducted among providers to assess for perceived barriers to care and knowledge of recommendations for initial visit. Post-intervention chart review was performed from 2022-2023 to determine if changes were made to provider practices.
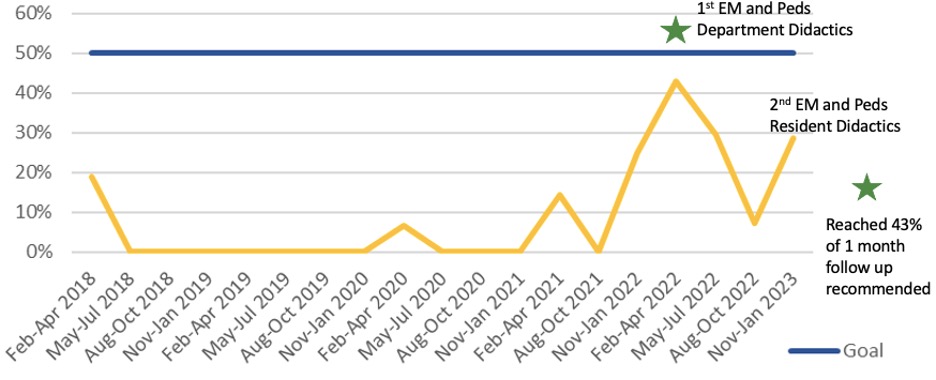
Results: Outcome goals were providing educational resources at 30% of encounters and recommending a follow-up timeframe of 1 month at 50% of encounters per AAP recommendation. After intervention, a near shift occurred with providers recommending 1 month follow-up increasing to 43%. Foster care specific patient education given increased from 0% to 29% after integration into EMR. Knowledge assessment on provider surveys regarding recommended follow-up timeframe increased from 63% to 82% after intervention. Providers’ self-reported knowledge of components of visits, documentation, and exam required being listed as a barrier to care decreased from 36% to 9% post-intervention. Other barriers remained similar, including lack of time, resources available, and communication with children’s division and foster parents.
Conclusion(s): Children in foster care represent a unique, vulnerable population with increased needs, though few healthcare providers feel comfortable caring for this population due to lack of knowledge in standards of care. Provider education and integration of auto-texts and foster parent resources into the EMR can improve provider comfort and appropriate patient referrals. Next steps include expanding education to other departments and creating sustained education for residents.
.jpg)
