Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 4: Nutrition in the NICU
451 - Frequency of Fluid Versus Nutrition Discussion on Rounds by Clinicians in Neonatal Intensive Care Units
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 451
Publication Number: 451.1846
Publication Number: 451.1846

Gustave H. Falciglia, MD, MSCI, MSHQS
Assistant Professor of Neonatology
Northwestern University
Chicago, Illinois, United States
Presenting Author(s)
Background: Fewer clinical decision support systems (CDSS) can calculate nutrition intake (energy or macronutrient) as compared to fluid intake. This support structure may influence clinicians in neonatal intensive care units (NICU) to prioritize discussion of fluid rather than nutrition intake.
Objective: To determine the frequency of discussion of fluid and nutrition intake during rounds in the NICU and whether frequency is associated with CDSS.
Design/Methods: We used an existing dataset created from surveys sent to clinicians at 34 NICUs affiliated with the Children’s Hospital Neonatal Consortium (CHNC). Surveys were sent to 3-4 clinicians at each NICU: CHNC physician site sponsor, dietitian, and other clinicians with an interest in nutrition. Respondents reported the presence of CDSS to calculate fluid and energy intake retrospectively (actual intake received in the past) and prospectively (estimated future intake based on orders), and the frequency (days per week: 0-7) clinicians discussed daily intake of: fluid (mL/kg); energy (kcal/kg); protein, fat, carbohydrate (g/kg). Discrepancies were resolved by phone or email. Frequency data were collapsed by NICU. Wilcoxon Signed Rank test compared the frequency of discussion for fluid intake to energy, protein, fat and carbohydrate intake. Mann Whitney U test compared the frequency of discussion of energy to fluid intake in NICUs with any CDSS to those without.
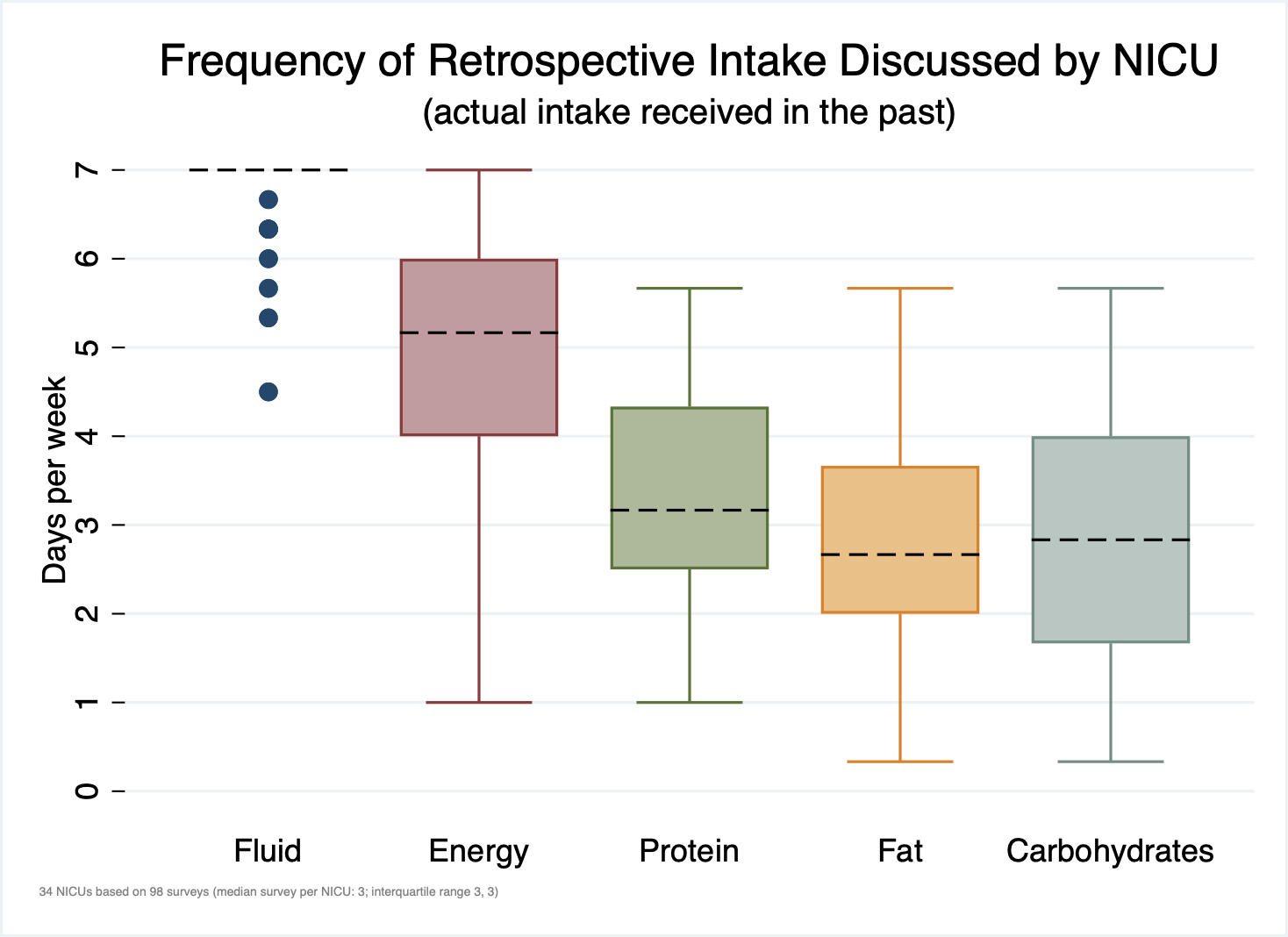
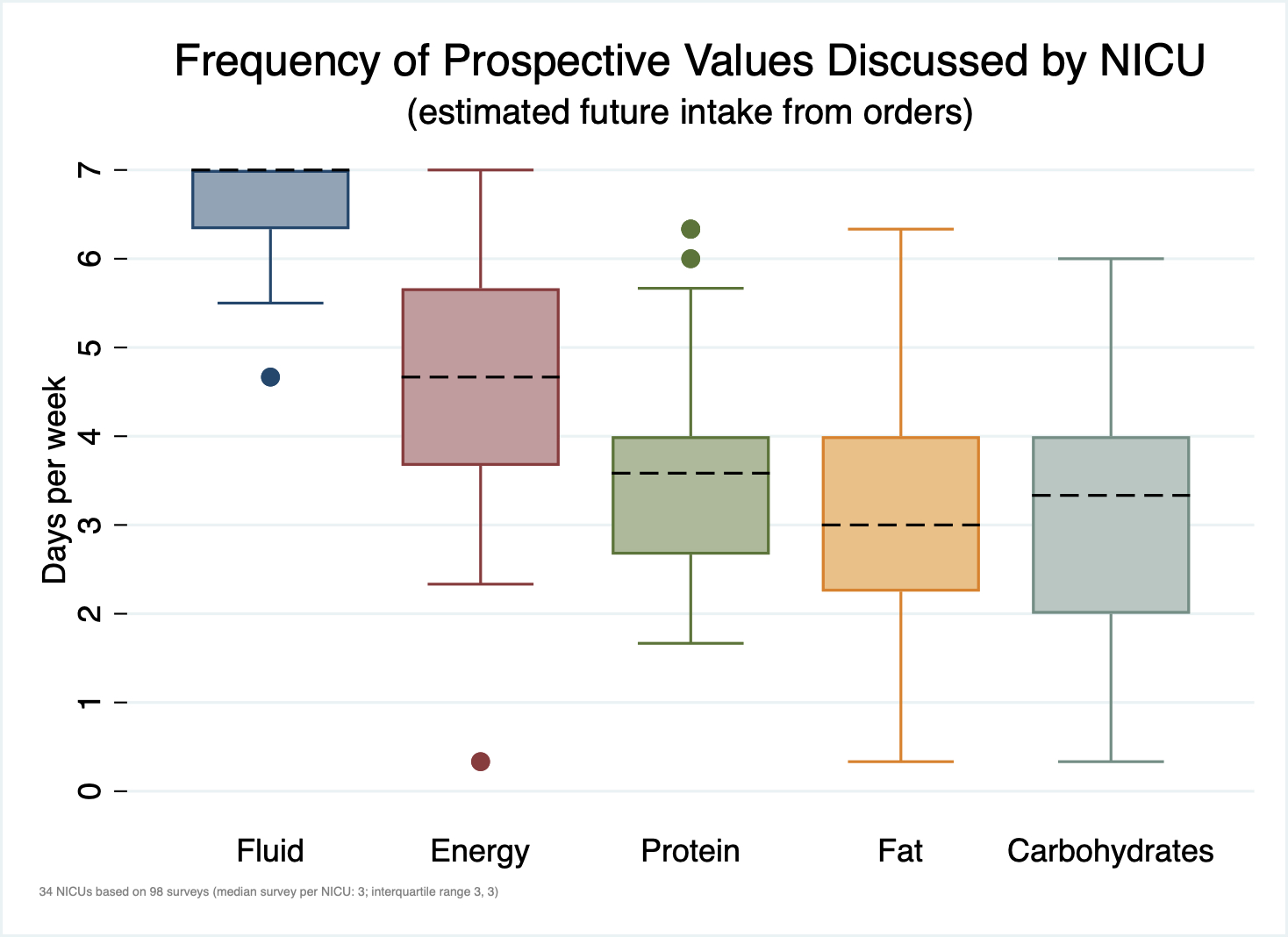
Results: Ninety-eight of 108 (91%) clinicians across all 34 NICUs completed the surveys. The median completed surveys per NICU was 3 (interquartile range: 3,3). Respondents were 57% neonatologists, 34% dietitians, 7% advanced practice providers and 2% pharmacists. Retrospective fluid intake was discussed more frequently than energy (p < 0.001), protein (p < 0.001), fat (p < 0.001) and carbohydrate (p < 0.001) intake (Figure 1). Prospective fluid intake was discussed more frequently than energy (p < 0.001), protein (p < 0.001), fat (p < 0.001) and carbohydrate (p < 0.001) intake (Figure 2). Though 11 (32%) NICUs had any CDSS to calculate retrospective nutrition intake only 1 (3%) had an automated CDSS that calculated intake from parenteral and enteral sources. There was no observed association between discussion frequencies and any CDSS.
Conclusion(s): Clinicians report discussions of retrospective and prospective fluid intake more frequently than energy or macronutrient intake. We speculate that there may be a greater focus on fluid intake rather than nutrition intake and that there are opportunities across NICUs to improve nutrition delivery.