Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
183 - Performance of the 2022 NICHD bronchopulmonary dysplasia (BPD) outcome estimator in identifying extremely preterm babies at risk of developing severe BPD in a single-centre UK study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 183
Publication Number: 183.3188
Publication Number: 183.3188
Georgina Yan, BSc MBChB (Hons) (she/her/hers)
Academic Clinical Fellow
University College London, England, United Kingdom
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) or death before 36 weeks postmenstrual age (PMA) is increasing in the UK, affecting 40% of babies born before 32 weeks gestation(1). It is associated with multisystem chronic morbidity and childhood mortality. We currently don’t have a prediction tool in the UK to identify babies at risk of developing severe BPD.
Objective: Our tertiary centre’s current practice is to consider postnatal steroids in babies who remain ventilated after day 14 of life. Our aim was to determine if the 2022 NICHD BPD outcome estimator (2) could identify which babies are likely to develop severe BPD on days 7 and 14.
Design/Methods: Our inclusion criteria matched the NICHD tool in birth gestation ( < 29 weeks), birth weight (501-1250g) and no major congenital anomalies. Infants were identified from an observational study (ClinicalTrials.gov Identifier: NCT05152316). The NICHD tool’s predictions based on clinical parameters on days 7 and 14 were compared to respiratory support requirement at 36 weeks PMA as per the 2019 classification. Severe BPD was defined as Grades 2 and 3 (requiring >2L oxygen per minute and/or positive pressure ventilation).
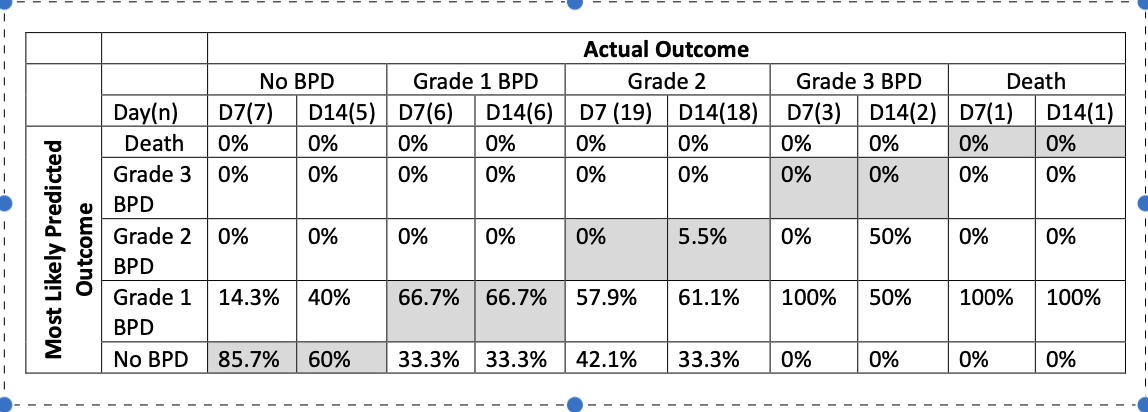
Results: 39 infants were included. Mean birth gestation was 26.4 weeks and mean birth weight was 807g. The tool had good sensitivity in predicting occurrence of BPD on day 7 (84.6%, n=33) and day 14 (92%, n=30). However, the tool under-predicted severity of BPD. On Day 7, for the 20 infants with severe BPD, it predicted 75% would only develop Grade 1 (mild) BPD and 25% would not develop BPD. On Day 14, it correctly predicted 5.9% (1/19) of Grade 2 BPD cases. Secondary analysis included babies on high-flow nasal cannula oxygen (using the continuous positive airway pressure mode in the tool). Specificity for grade of BPD remained poor (Table 1).
Conclusion(s): The 2022 NICHD tool had good sensitivity in predicting occurrence of BPD in our infants but was poor at predicting severe disease. The ability to identify babies at risk of severe BPD is important for calculating risk and benefit of postnatal therapies such as steroids and in prognosis counselling. Research is needed to delineate the roles of other factors in evolving BPD including current ventilation practices, intrauterine growth restriction and undernutrition.
With many thanks to research nurses Vera Grenha, Kathy Chant and Laura Holmes.
(1) National Neonatal Audit Programme 2022 Data: Extended Analysis Report. RCPCH: London.
(2) Greenberg RG, et al (2022) Online clinical tool to estimate risk of bronchopulmonary dysplasia in extremely preterm infants Arch Dis Child Fetal Neonatal Ed 107:F638–F643