Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
77 - Perinatal Factors Associated with Successful Pharmacologic Closure of the Patent Ductus Arteriosus in Preterm Infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 77
Publication Number: 77.1864
Publication Number: 77.1864

Puneet Sharma, MD
Clinical Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: The patent ductus arteriosus (PDA) is associated with significant morbidity and mortality in preterm infants. While many clinicians elect for pharmacologic closure to abate this risk profile, not every patient responds. If clinicians knew which factors were associated with successful pharmacologic closure, it could allow them to anticipate the need for procedural closure and minimize delays in care.
Objective: To determine which perinatal factors are associated with successful pharmacologic closure of the PDA.
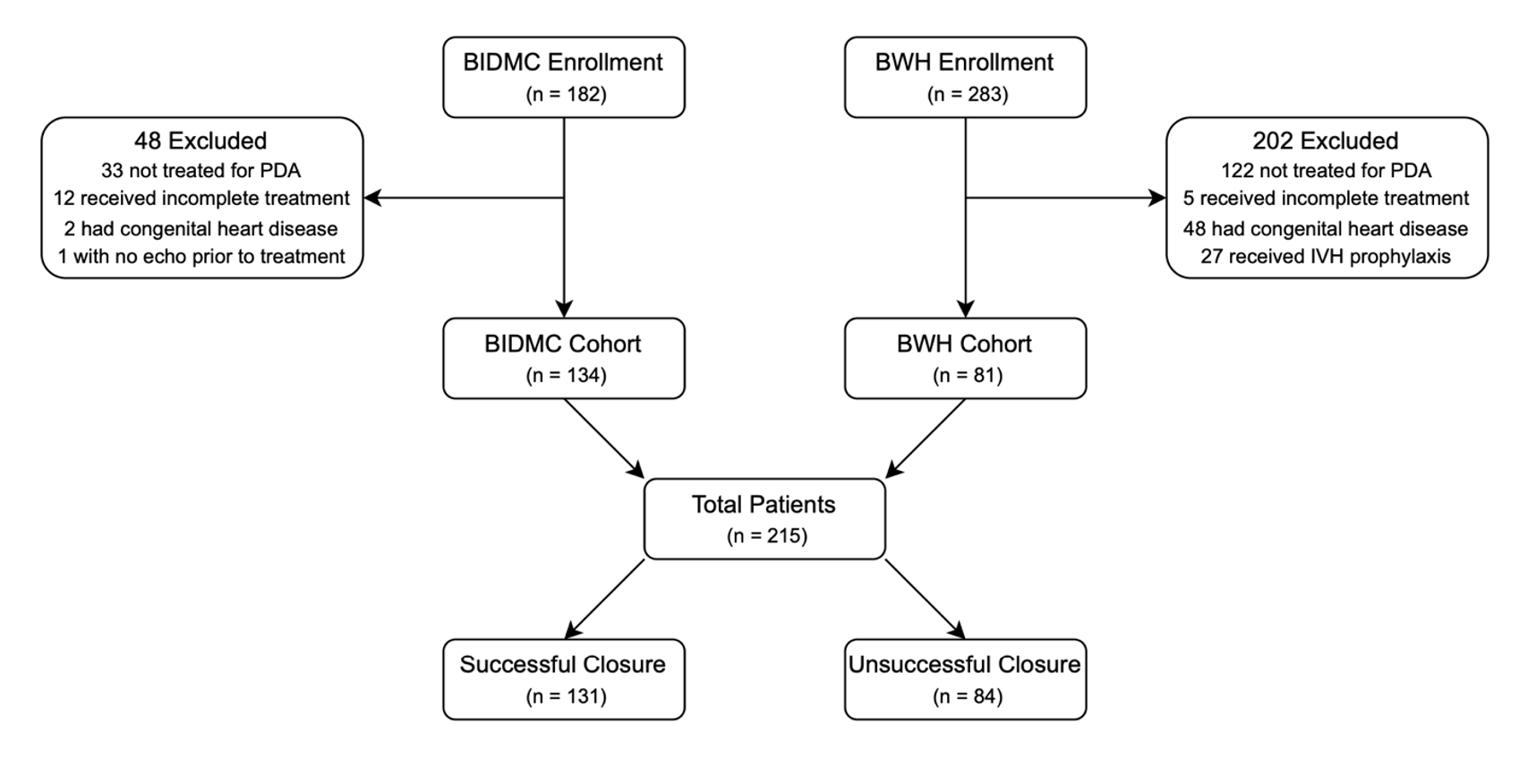
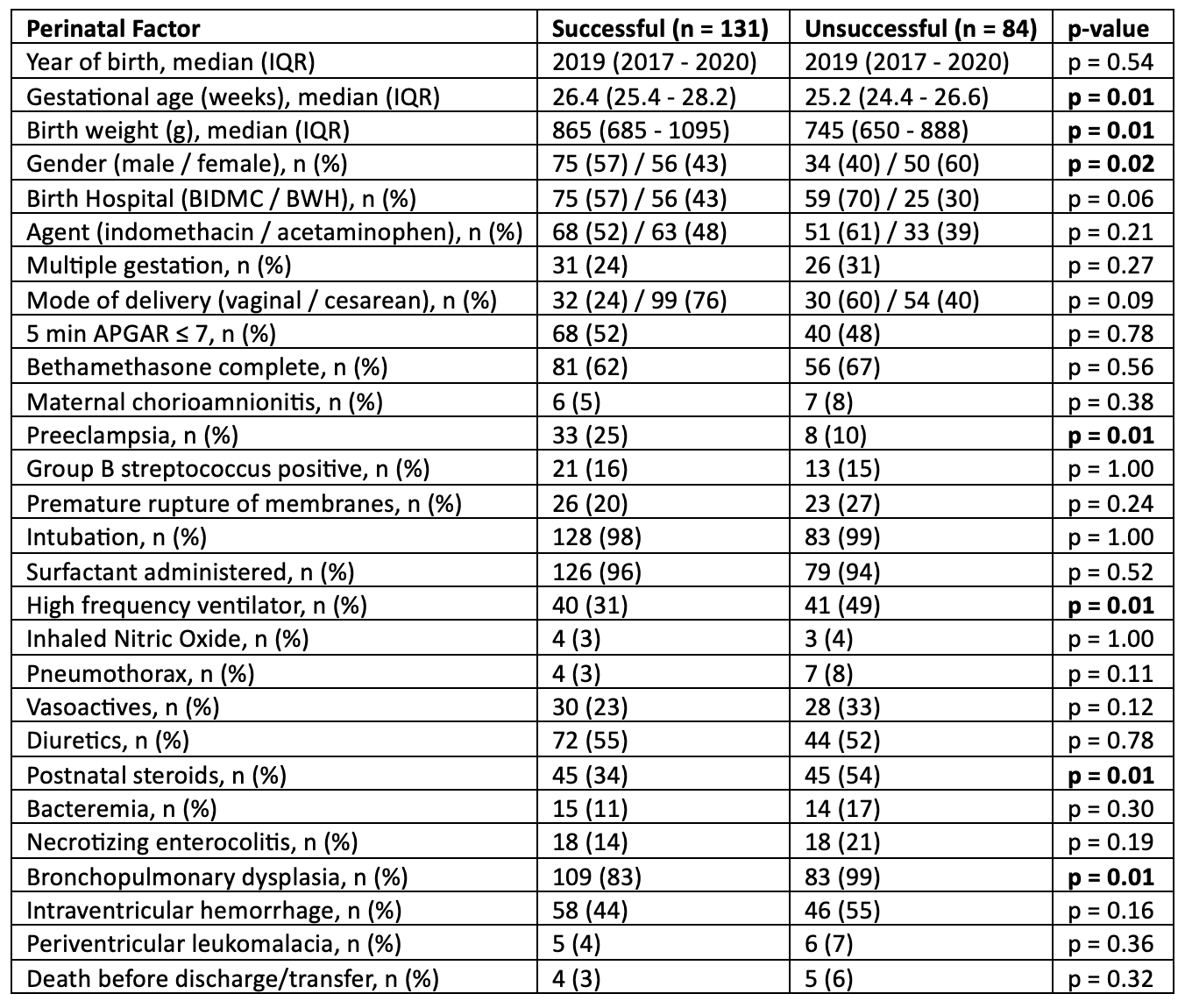
Design/Methods: We performed a 5-year retrospective cohort analysis of preterm infants (born < 37 weeks gestation) who received pharmacologic treatment (indomethacin or acetaminophen) for a PDA at two large Boston neonatal intensive care units (Beth Israel Deaconess Medical Center (BIDMC) and Brigham and Women’s Hospital (BWH)) between January 2016 and December 2021. Infants were excluded if they received prophylactic indomethacin, had early termination of therapy, did not have an echocardiogram prior to therapy, or had congenital heart disease. The primary outcome was successful closure of the PDA, defined as no additional courses of pharmacotherapy or procedural closure. Relevant perinatal data were collected to identify which factors were associated with successful closure. Fisher’s exact test was performed on categorical variables while Mann-Whitney U test was performed on continuous variables.
Results: We identified 215 infants who received pharmacologic treatment for their PDA. 131 infants had successful closure (61%) with no significant difference in success rate at either hospital. The success rate of pharmacologic closure in our cohort was consistent with current literature. Older gestational age at birth (p = 0.01), higher birth weight (p = 0.01), male sex (p = 0.02), and maternal pre-eclampsia (p = 0.01) were associated with successful closure. Infants with unsuccessful closure were more likely to require high-frequency ventilation (p = 0.01), require postnatal steroids (p = 0.01), and develop bronchopulmonary dysplasia (BPD) (p = 0.01).
Conclusion(s): We demonstrated an association between gestational age, birth weight and success of closure, consistent with the literature. The association of successful closure with male sex and maternal pre-eclampsia is novel and warrants further investigation. The association between high-frequency ventilation, postnatal steroids for lung disease, and bronchopulmonary dysplasia (BPD) and unsuccessful pharmacologic closure is concerning and also requires further exploration.