Health Services Research
Session: Health Services Research 3: Access
227 - Diseases of Childhood in Adolescence and Beyond: Implications for the Management of Comorbidity
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 227
Publication Number: 227.1792
Publication Number: 227.1792

David Chartash, PhD
Lecturer
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Children are not little adults. This central tenet of pediatrics lays an important foundation for the care of children. However,
children do become adults. Understanding the complexities of that transition is important for pediatricians prior to handover to adult physicians.
In particular, more data is needed on how the prevalence of common co-occurring conditions changes with age.
Objective: To assess variations in comorbidities by age in order to inform the development of a standard metric of patient complexity for children and
adolescents similar to the Elixhauser index developed for adults. We selected six diagnoses to highlight how comorbidities influence on patient risk changes with age.
Design/Methods: A retrospective observational cohort study was performed on all primary care and hospital visits between 2013 and 2022 at an academic urban medical in the Northeastern United States. Using ICD-10CM, RxNorm, CPT, and LOINC codes taken from patient visits we used word2vec to create
patient embeddings, and ordering these embeddings by patient age, we constructed a phase space of patient health status. The false nearest neighbor (FNN) algorithm and transitivity based analysis described by Neuman et al [1] were used to identify transitions in patient healthcare found in his phasespace. We then used the patients in the intervals between the transition points to create comorbidity indices for each interval based on the same method used in the Elixhauser index: ordinary least squares regression for logged length of stay.
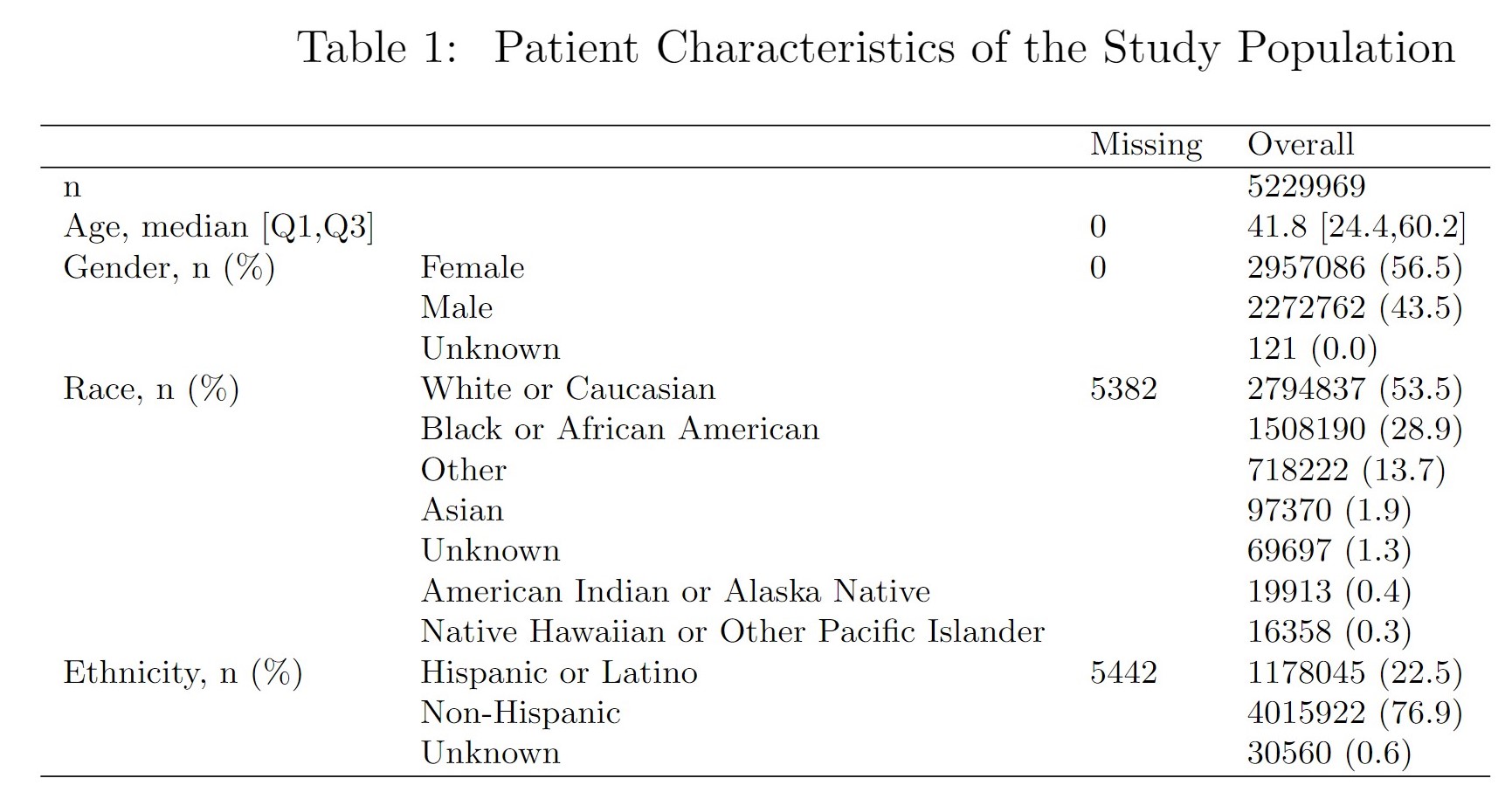
Results: We used over 5.2 million patient encounters as described in Table 1. The coefficients of the novel comorbidity index based on FNN and Transitivity intervals are shown in Figure 1a and Figure 1c. The forest plot showing the confidence intervals of regression coefficients are shown in Figure 1b and Figure 1d. We find that psychosis and complicated diabetes observes a greater risk impact in children than adults (particularly for children below age 7), while complicated hypertension has a greater and less variable risk impact in adults (particularly older adults).
Conclusion(s): Most comorbidity indices are constructed using primarily adult populations. Highlighting six diagnoses, we found specific areas where comorbidity
indices should be adjusted in the pediatric context compared to adults, reinforcing the need for unique indices for children. Additionally, due to the rapid changes in patients physiology at young ages, unique indices are needed for individual cohorts within the conventional 0-18 pediatric age range.
[1] 10.1371/journal.pone.0101014
.png)
