Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 2: Human Milk Feeding
481 - Improving intake of mother’s own milk in a large, urban neonatal intensive care unit (NICU)
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 481
Publication Number: 481.1788
Publication Number: 481.1788

Keadrea Wilson, MD (she/her/hers)
Assistant Professor of Pediatrics, Division of Neonatology
UTHSC
Memphis, Tennessee, United States
Presenting Author(s)
Background: Mother’s own milk (MOM) is the optimal nutrition for all infants, but especially those born < 1500g or very low birth weight (VLBW) infants because it lowers the risk of many prematurity-related complications. Despite the benefits, at Regional One Health (ROH) in Memphis, TN, the percentage of VLBW infants receiving MOM at discharge remains low. We implemented a multidisciplinary lactation improvement team to promote higher provision of MOM among VLBW infants.
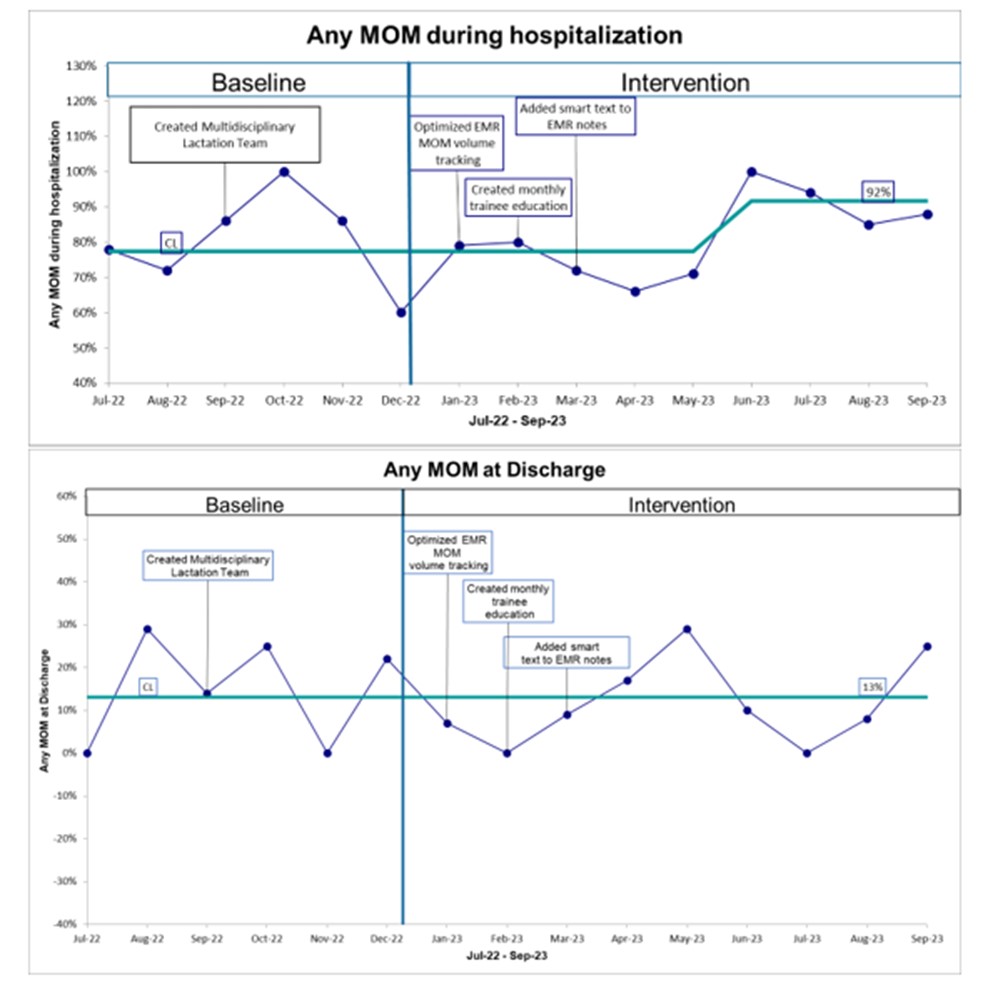
Objective: We aimed to increase the percentage of all VLBWs receiving any MOM at discharge from 22% to 24% by December 2023 as an intermediate aim and from 22% to 32% by December 2024 as a stretch aim. Secondly, we aimed to increase the percentage of all VLBWs receiving any MOM during hospitalization from 80% to 88% by December 2023 by intermediate aim and from 80% to >90% by December 2024.
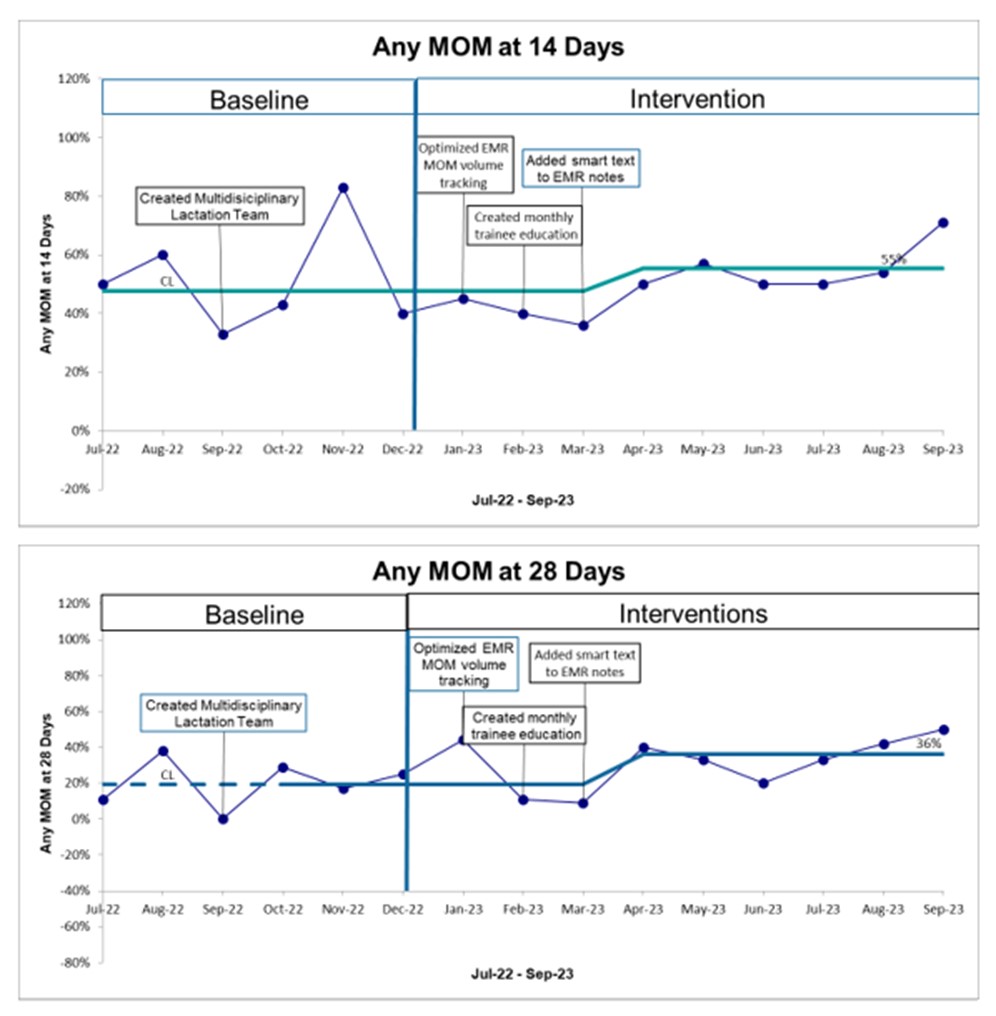
Design/Methods: At ROH, we established a multidisciplinary team of lactation consultants, labor & delivery and neonatal intensive care unit (NICU) nurses, dieticians, doctors and nurse practitioners. Baseline data was obtained from July to December 2022. The primary outcome measures were % any MOM at discharge and the % any MOM during hospitalization. Intermediate measures included % any MOM at 14 days and 28 days. Plan-do-study-act cycles included organizing a multidisciplinary lactation team, creating MOM tracking in the electronic medical record (EMR), developing trainee education on breastfeeding in the NICU and adding MOM education smart text to provider notes. Statistical process charts were used.
Results: The center line of those receiving any MOM during hospitalization showed an increasing trend although no run was noted. Also, the percentage of VLBW infants who received any MOM at 14 days and at 28 days each showed a cumulative increase as the centerline shifted up from 48% to 55% and 20% to 36%, respectively. There was no shift upward or downward in MOM at discharge compared to the baseline average.
Conclusion(s): Our quality improvement interventions increased the overall percentage of VLBW infants who had any MOM during hospitalization. We also observed an increase in the intermediate measure of MOM at 14 days and 28 days while maintaining the percentage of infants receiving MOM at discharge. These interval gains reveal an opportunity for further targeted efforts during the first month of life where risk of necrotizing enterocolitis is highest and in which mothers establish their milk supply and enable prolonged provision of breast milk even until discharge.