Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 2: BPD and prematurity
92 - Feasibility of 3D-Echocardiography for LV performance and dimensions in the immediate postnatal neonatal period – a prospective study.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 92
Publication Number: 92.1797
Publication Number: 92.1797

Sariya Sahussarungsi, MD (she/her/hers)
Fellow
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Presenting Author(s)
Background: There is a paucity of data regarding 3D-echocardiography derived parameters of left ventricular (LV) dimensions and function in the neonatal population. Neonates are potential good candidates for the 3D-echocardiography technology, as they often allow for high quality resolution by ultrasound, secondary to their easily achievable acoustic windows. 3D-echocardiography (ECHO) may be used to uncover subtle changes in cardiac performance, allowing for the comparative normative values to evaluate at-risk infants.
Objective: Our primary objective was to evaluate the feasibility of obtaining 3D-echocardiography in the immediate post-natal neonatal period and to obtain parameters of cardiac function and dimension in healthy newborns, within the first 48 hours of life. Our secondary objective were to evaluate if age at echocardiography (in hours), sex or birthweight could influence these parameters.
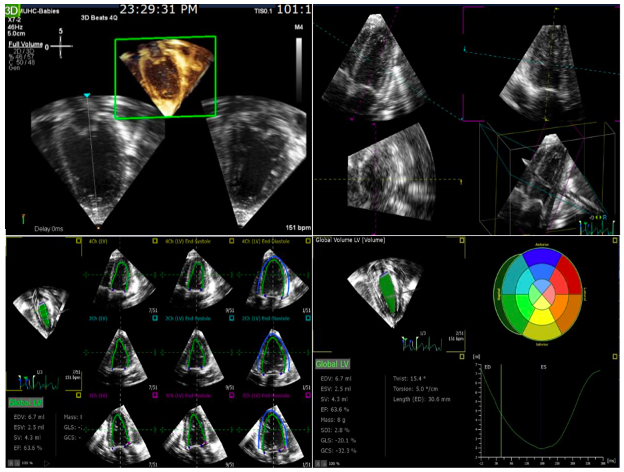
Design/Methods: Prospective observational study recruiting healthy newborns born after an uneventful pregnancy, without resuscitation. After consent, ECHO using the X2-matrix probe and Philips Epiq7 was performed by trained professionals. A blinded rater extracted off-line LV parameters using Speckle-tracking ECHO (STE) with TomTEC Arena. Descriptive statistics and regressions were used to analyze the data.
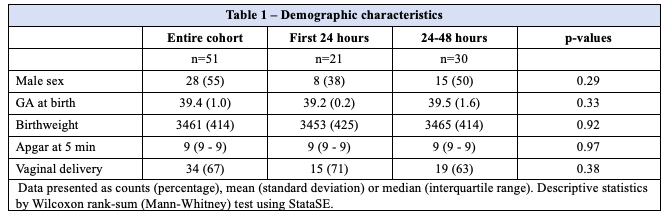
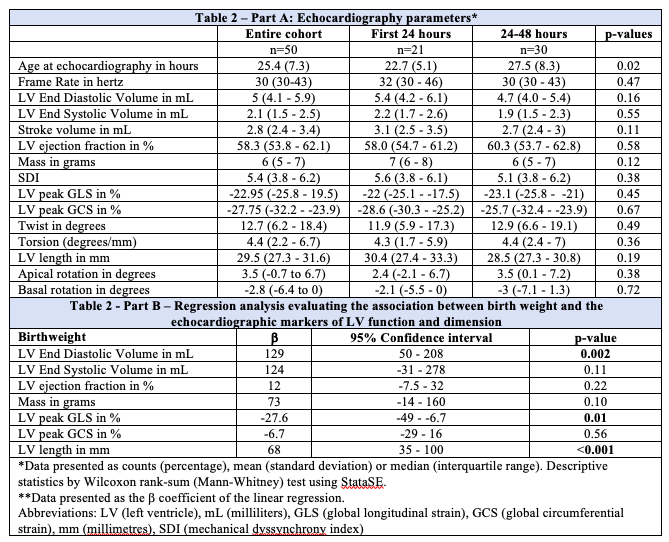
Results: We prospectively enrolled 51 newborns, out of which 28 (55%) were male. These infants were born at term, with a mean gestational age of 39.4 weeks (±1.0). Echocardiography was performed close to 24 hours of life. No differences were noted between those that were evaluated prior or after 24 hours of life. Echocardiography (3D) and analysis by STE was feasible in 50 infants (98%). Markers of LV volumes and function are presented in Table 2. No differences were found based on sex. By linear regression, birthweight was associated to the LV end-diastolic volume (p=0.002) and LV length (p < 0.001) (increasing dimensions corresponding to increasing birthweight), but not to their LV ejection fraction. Birthweight was associated to cardiac longitudinal deformation (GLS: p=0.01), a marker of LV contraction, but not to circumferential deformation (GCS: p=0.56).
Conclusion(s): We here demonstrate the feasibility of assessing the LV dimensions and function of neonates using 3D-echocardiography, during their transitional period. We found an association between certain markers of function and dimensions and the neonate’s birthweight. As expected, LVEDd and LV length correlate with body weight. Interestingly, while longitudinal deformation is associated with body weight, circumferential deformation is not.