Immunizations/Delivery
Session: Immunizations/Delivery 1
33 - COVID-19 Pandemic Impact on Uptake of Select Required Adolescent Vaccines in the U.S. Military Health System
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 33
Publication Number: 33.1538
Publication Number: 33.1538
.jpg)
Sohyun Ha, DO (she/her/hers)
Pediatric Resident Physician
Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine
Chesapeake, Virginia, United States
Presenting Author(s)
Background: During the COVID-19 pandemic, access to well-child care and vaccinations was significantly disrupted. Additionally, a rise in vaccine hesitancy has hampered vaccine uptake. Human papillomavirus (HPV), tetanus, diphtheria, and acellular pertussis (Tdap), and tetravalent meningococcal conjugate (MCV4) vaccines are each required to attend school in some U.S. States. Department of Defense (DoD) beneficiaries have universal access to these vaccines, however, disparities in this population remain.
Objective: We aimed to evaluate pandemic-related trends in HPV, Tdap and MCV4 vaccine uptake among adolescent DoD beneficiaries to identify the optimal groups and locations for targeted vaccination strategies.
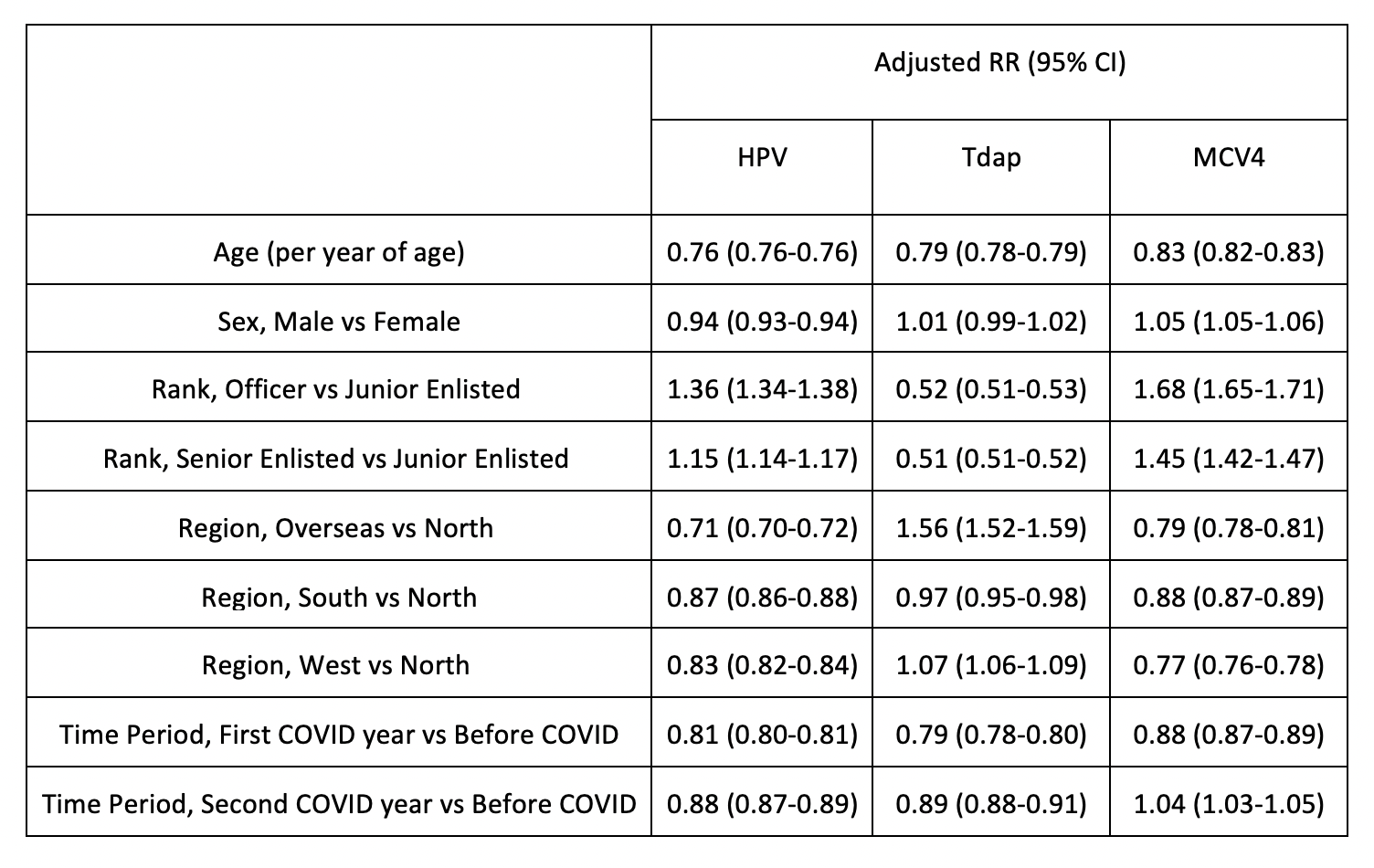
Design/Methods: We completed a retrospective repeated monthly cross-sectional study utilizing data from TRICARE Management Activity’s Military Health System (MHS) Database. DoD beneficiaries 11 to < 22 years of age enrolled in TRICARE in any month from March 2018 to February 2022 were included. HPV, Tdap, and MCV4 vaccinations administered during this period were identified using Current Procedural Terminology codes and used to calculate monthly vaccination rates. Adjusted Poisson regression was used to estimate vaccination rate ratios according to time period (Before COVID – Mar 2018 to Mar 2020, First COVID Year - Mar 2020 to Mar 2021, Second COVID Year - Mar 2021 to Feb 2022), age, sex, sponsor rank, and geographic region.
Results: Adolescent median monthly vaccination rates for HPV and Tdap were 12% and 11% lower respectively in the second COVID year compared to the pre-pandemic years. In contrast, rates of MCV4 vaccination in adolescents were 4% higher in the second COVID year than before the pandemic. Across the entire study period vaccination rates for HPV and MCV4 were 36% and 68% higher respectively among adolescent children of officers compared to junior enlisted service members and were higher in the North region. Vaccination rates for all vaccines were similar between male and female adolescents and followed a seasonal pattern with peaks each August.
Conclusion(s): Despite universal access to healthcare in the MHS, vaccination rates for HPV and Tdap in adolescents have not yet recovered to pre-pandemic norms. Additionally, vaccination rates for HPV and MCV4 are substantially lower among dependents of enlisted servicemembers, and those living in regions other than the North, highlighting potential education gaps, healthcare disparities, or both. Next steps are to assess attitudes toward and barriers to vaccination in these groups and provide them targeted vaccine education and allocation.
.png)
.png)
