Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
355 - The Dosing Weight Waltz: Improving Pediatric Dosing Weight Accuracy on Inpatient Units
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 355
Publication Number: 355.1727
Publication Number: 355.1727

Ann Kane, MD (she/her/hers)
Medical Director of Quality
Johns Hopkins Children's Center
Silver Spring, Maryland, United States
Presenting Author(s)
Background: Medication errors related to inaccurate dosing weights can create opportunities for harm to patients. Using inaccurate estimated or stated weights for medication or fluid dosing longer than medically necessary was identified as a contributing factor in medication errors at our institution.
Objective: The goal of this study was to decrease the timing of when an estimated weight is used as a dosing weight before a measured weight is obtained. Baseline data indicated only 17.6% of our patients have a measured weight within 12 hours of admission to an inpatient unit. Our goal was to improve patients having a measured weight within 12 hours of admission to 75% within 6 months.
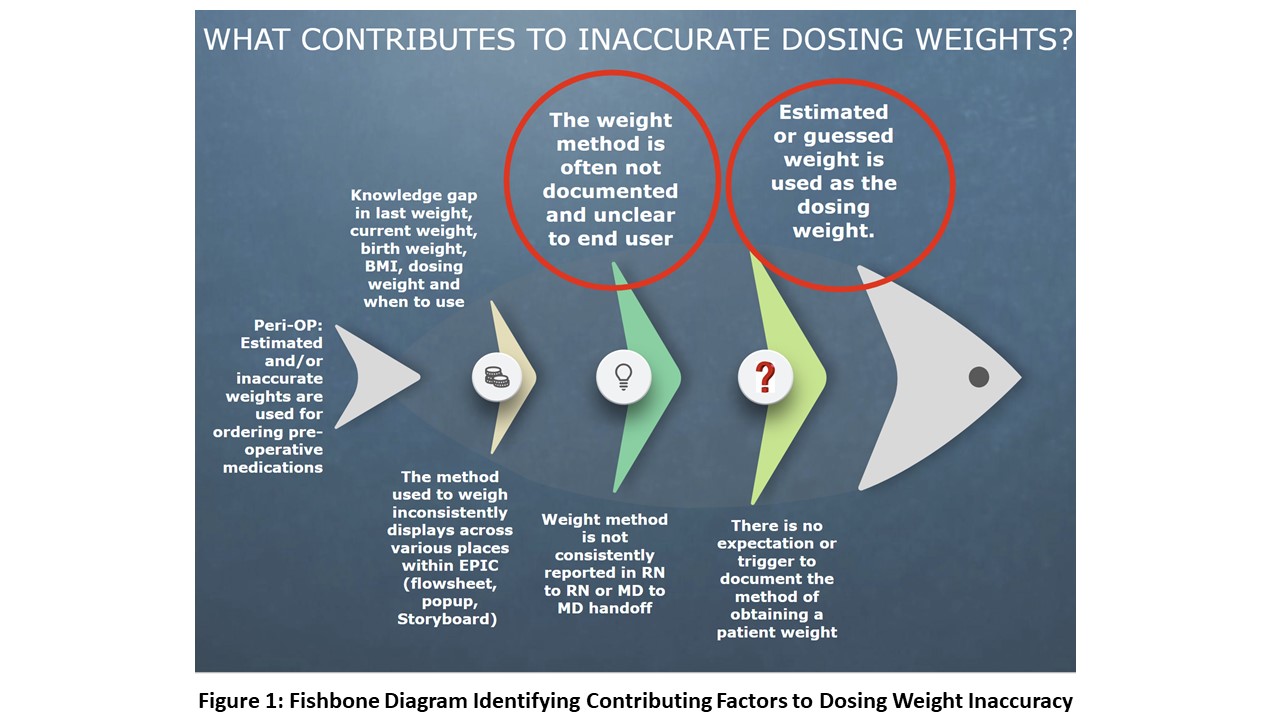
Design/Methods: Scope included all units except the neonatal ICU. Baseline data was collected between 9/2020-11/2021. Prior to interventions, a work group was formed to reveal root causes for dosing weight inaccuracies. Figure 1 demonstrates the fishbone diagram. PDSA cycle 1 (12/2021-3/2022) was an educational campaign to promote documentation of weight ‘method’ used. We then made several changes to the electronic medical record (EMR) including 1. Require weight method documentation for inpatient encounter (PDSA 2; 3/2022) 2. Adding weight method row to nursing task list and increased visibility of dosing weight in EMR (PDSA 3; 6/2022) 3. Require weight method documentation in the pediatric emergency department (PDSA 4; 8/2022).
Results: Figure 2 demonstrates a P chart with the proportion of measured weights obtained within 12 hours of admission. After PDSA cycles 1-4, measured dosing weights improved from a baseline of 17.6% to 67.5%, noting a special cause variation shift in the data. Figure 3 demonstrates an I chart with a reduction of individual encounters with dosing weight method not documented. Performing a one-way ANOVA showed a statistically significant difference between the means of the baseline data and PDSA cycles 1-4 in the number of inpatient encounters with weight method not documented (p < 0.000). Testing for equal variances also revealed a statistically significant reduction in the variance in the number of inpatient encounters with weight method not documented (p < 0.000).
Conclusion(s): We saw significant improvement of accurate measured dosing weights obtained during hospital admission and continue to see sustained improvements over time, however we have yet to meet our initial goal of 75%. Future directions include adding an EMR nursing best practice alert as a reminder to obtain a measured weight as well as update hospital policy on required adherence to obtain a measured dosing weight upon admission.
.jpg)
.jpg)
