Emergency Medicine
Session: Emergency Medicine 7: Emergency Medical Services
212 - Test characteristics of age-adjusted vital sign abnormality thresholds to predict in-hospital outcomes among children transported by emergency medical services
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 212
Publication Number: 212.1720
Publication Number: 212.1720
- SR
Sriram Ramgopal, MD (he/him/his)
Assistant Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Prehospital pediatric vital signs parameters are commonly used to guide treatment interventions, direct patients to pediatric specialty centers, and activate hospital processes. Empirically derived vital signs criteria may provide a meaningful way to children at risk of serious injury or illness.
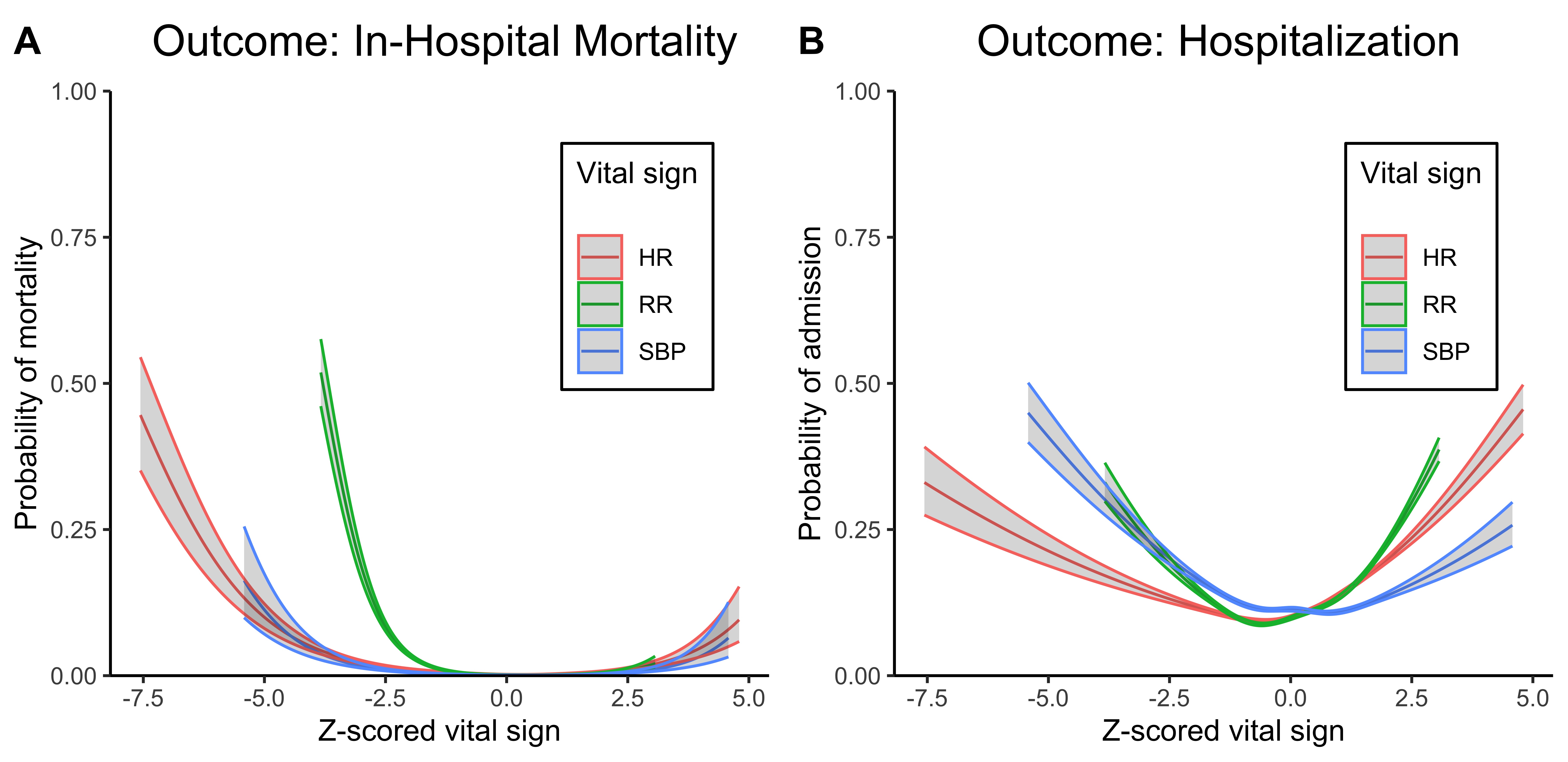
Objective: To evaluate the association between empirically derived cutoffs and Pediatric Advanced Life Support (PALS) cutoffs with outcomes of in-hospital mortality and hospitalization.
Design/Methods: We performed a retrospective, multi-agency study using deidentified prehospital patient care records from a large emergency medical services (EMS) electronic health record vendor in the United States. We included children ( < 18 years) transported by EMS from the scene with available in-hospital outcome data between 2018-2022. Our outcomes were in-hospital mortality and hospitalization. Our predictor of interest was initial vital signs, classified using two sets of empirically-derived age-adjusted criteria (higher-sensitivity and higher-specificity criteria) for predicting the receipt of potentially lifesaving prehospital interventions; Table 1) and PALS vital signs criteria. We assessed the diagnostic accuracy and performed univariable logistic regression to identify the association between abnormal vital signs and outcomes.
Results: Among 187,336 pediatric transports, hospitalization occurred in 23,338 (12.5%) and in-hospital mortality occurred in 1,166 (0.6%). All vital signs were associated with both outcomes (Figure 1). When using higher-sensitivity criteria, accuracies ranged from 28.5 to 43.5% with specificities of 28.3 to 42.3%. When using higher-specificity criteria, accuracies ranged from 74.3 to 92.9% with sensitivities of 37.4 to 41.9%. When using PALS criteria, accuracies ranged from 56.1-82.7%. The PALS criteria for heart rate and systolic blood pressure performed similarly to the higher-sensitivity criteria. The PALS respiratory rate criteria performed similarly to the higher-specificity criteria. The higher-specificity criteria for respiratory rate were associated with the greatest odds of mortality (Table 2). Findings were similar for hospitalization, but with smaller effect sizes.
Conclusion(s): The use of vital sign cutoffs derived from children receiving prehospital care and paired to clinically important outcomes may allow for improved prediction of critical illness for children transported to the hospital.
.png)
.png)
