Emergency Medicine
Session: Emergency Medicine 6: Airway and POCUS
199 - Novel approach to rapid quantitative evaluation of cardiac function in pediatric patients with normal cardiac anatomy
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 199
Publication Number: 199.1693
Publication Number: 199.1693
.jpg)
Elena Chen, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
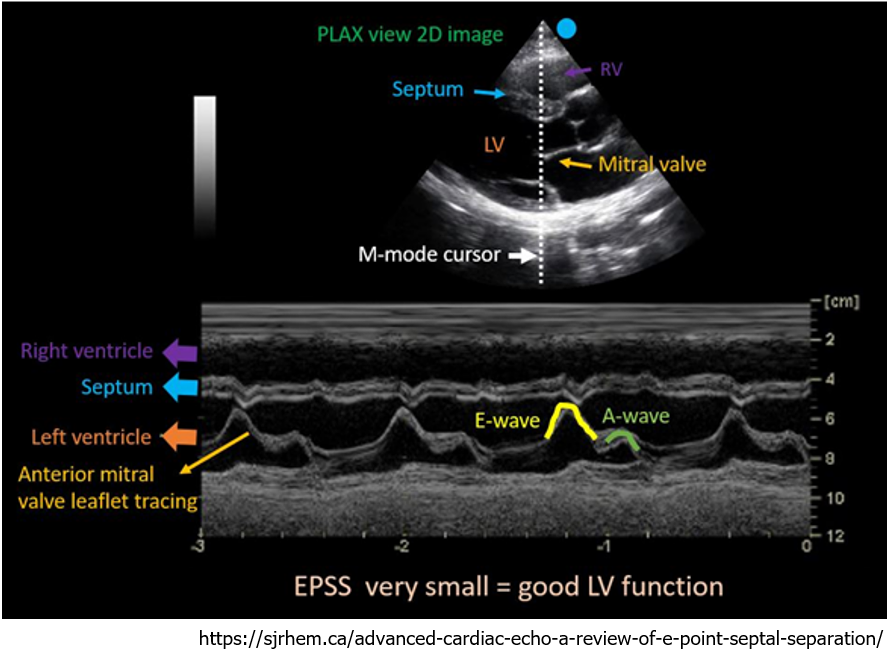
Background: Cardiogenic shock is an infrequent but important cause of morbidity in children. Point of care ultrasound (POCUS) can serve an important role in identifying the presence of heart failure in a child with undifferentiated shock. E-point septal separation (EPSS), defined as the distance from the mitral valve leaflet to the interventricular septum in early diastole, is a useful technique to screen for left heart failure. The utility of EPSS in screening for left ventricular failure among children is not established.
Objective: To (1) evaluate the distribution of EPSS in children, (2) determine if there is an association between EPSS and cardiac dysfunction, and (3) identify a clinically meaningful EPSS cutoff to screen for cardiac dysfunction in pediatric patients.
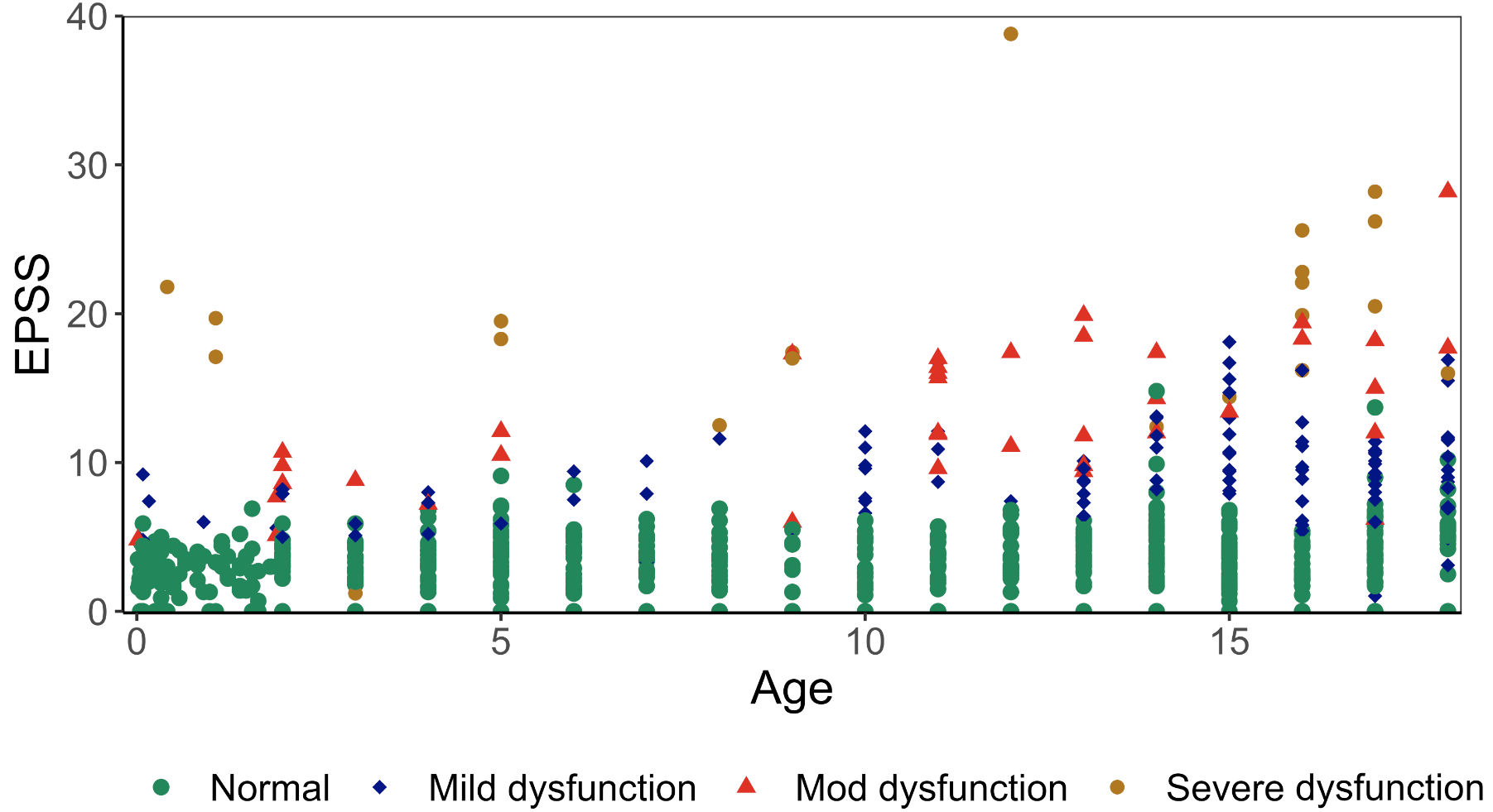
Design/Methods: We performed a single center, retrospective study of children ( < 18 years) who received an echocardiogram between 2019-2022, excluding children with congenital heart disease and mitral valve and interventricular septal abnormalities. Studies were categorized into normal and abnormal cardiac function based on either fractional shortening or left ventricular ejection fraction. A random sampling of 11,795 echocardiograms were measured by a study investigator blinded to echocardiogram results (Figure 1). We evaluated the age-based distribution of EPSS among included patients. We compared EPSS measurements between children with and without cardiac dysfunction using the Wilcoxon rank-sum test. We evaluated the diagnostic accuracy of the EPSS measurement when using a cutoff of 7mm for outcomes of mild, moderate, and severe dysfunction as defined by the modified Ross criteria.
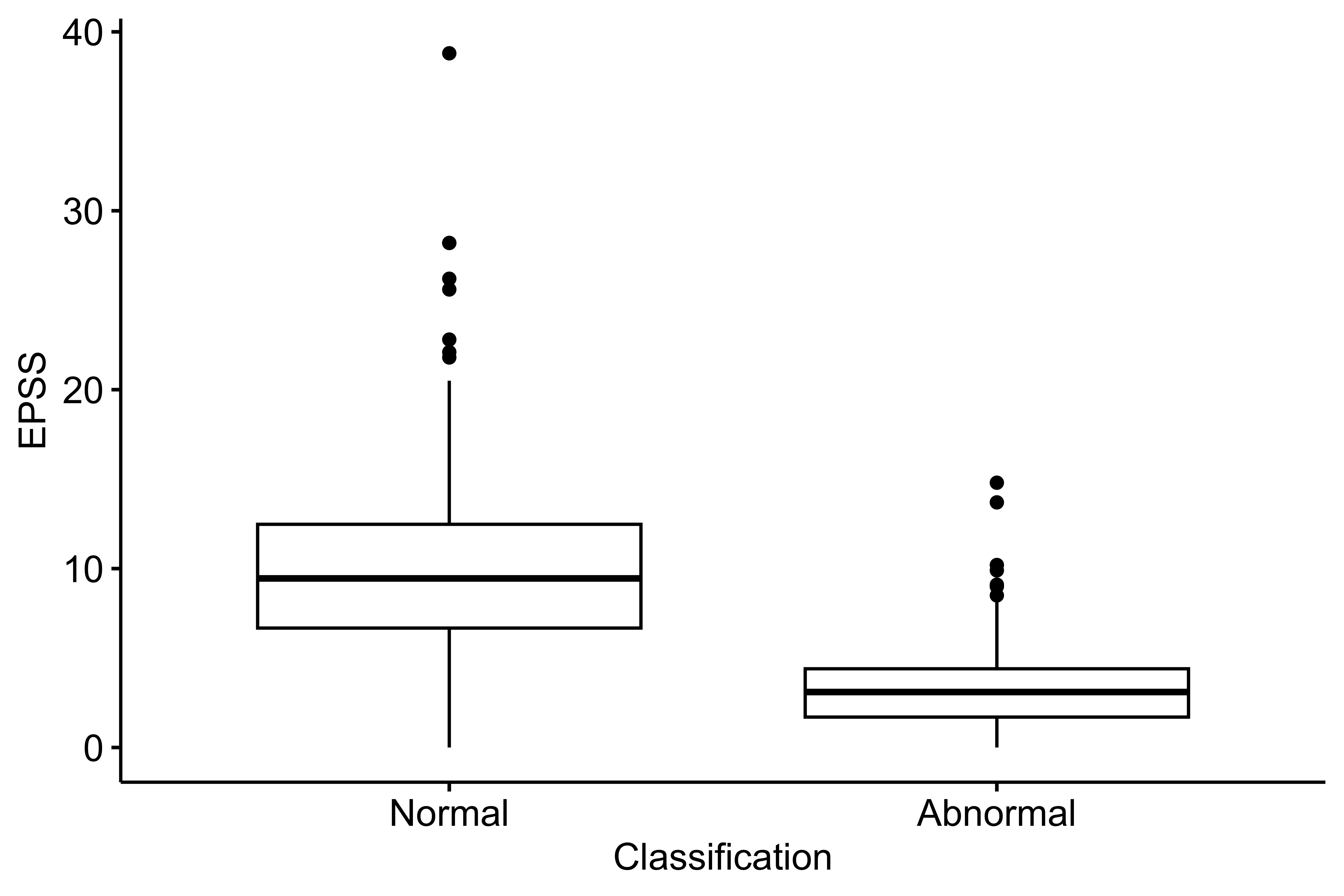
Results: We included 795 studies including 600 with normal function, and 133, 40, and 22 with mild, moderate, and severe dysfunction, respectively. EPSS measurements rose with increasing age (Figure 2). EPSS measurements were higher among children with abnormal cardiac function (p < 0.01; Figure 3). Using a 7mm cutoff resulted in a 95% sensitivity and 84% specificity for severe dysfunction, 92% sensitivity and 88% specificity for moderate-severe dysfunction, and a 71% sensitivity and 98% sensitivity for any cardiac dysfunction.
Conclusion(s): EPSS measures increase during early childhood before reaching adult values. EPSS correlates with cardiac dysfunction in children. A cutoff value of 7mm also seems to be an adequate screen for moderate to severe dysfunction with a sensitivity of 92%, though a lower cutoff may have greater utility in younger age groups.