Emergency Medicine
Session: Emergency Medicine 12: Potpourri
427 - Examining Neighborhood Opportunity and Delays to Presentation and Imaging Among Children Presenting to the Emergency Department with Stroke-like Symptoms
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 427
Publication Number: 427.3335
Publication Number: 427.3335

Laura N. Wilson, MPH (she/her/hers)
Medical Student
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Pediatric strokes are rare but can greatly affect morbidity and mortality in children. Timely diagnosis is crucial, but research suggests pediatric strokes are often diagnosed with substantial delays. Composite scores of neighborhood opportunity, such as the Childhood Opportunity Index (COI), have been utilized to assess how limited resources in one’s neighborhood delay the diagnosis and treatment of certain conditions, but no such variable has been examined in the context of pediatric strokes.
Objective: The primary objective was to assess if neighborhood opportunity, as defined by the COI, is predictive of time to presentation (TTP) among children with stroke-like symptoms. The secondary objective was to identify predictors of delays in door-to-imaging time (DIT) within the emergency department (ED).
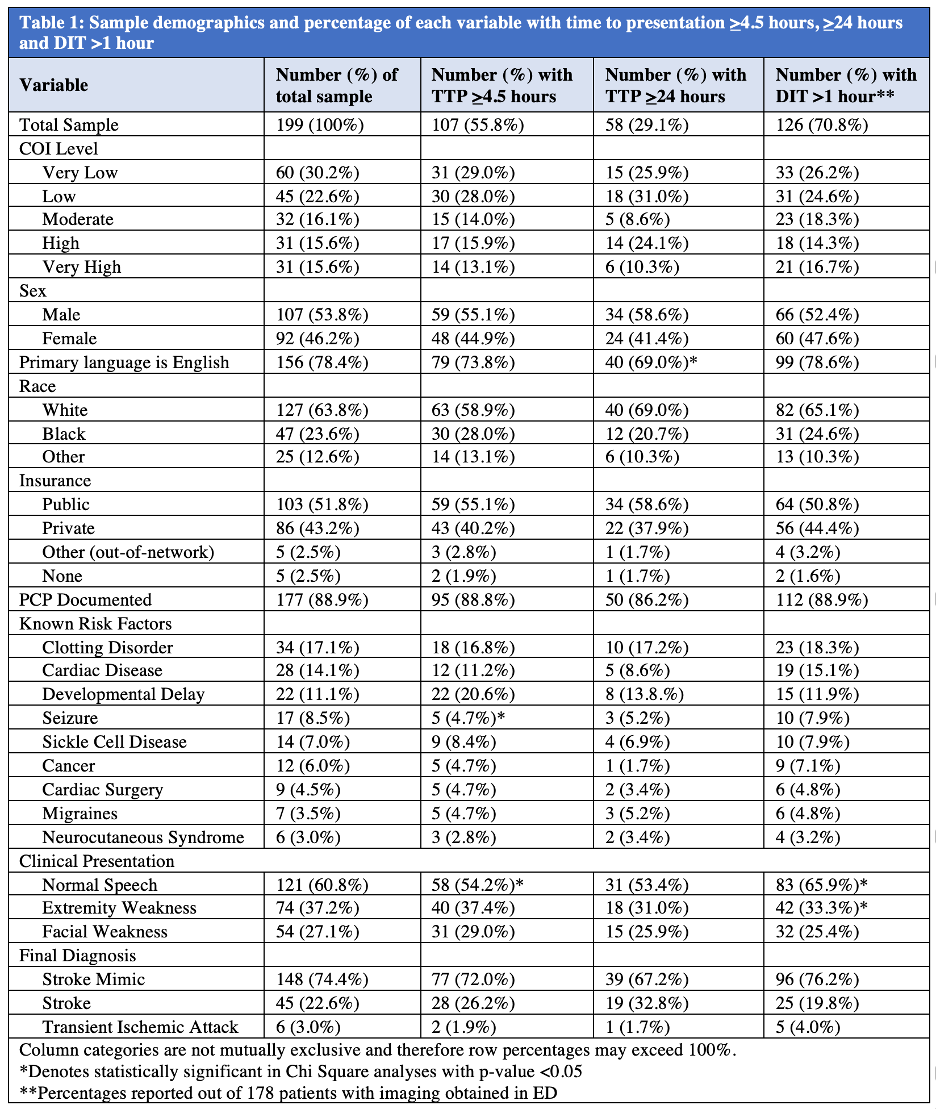
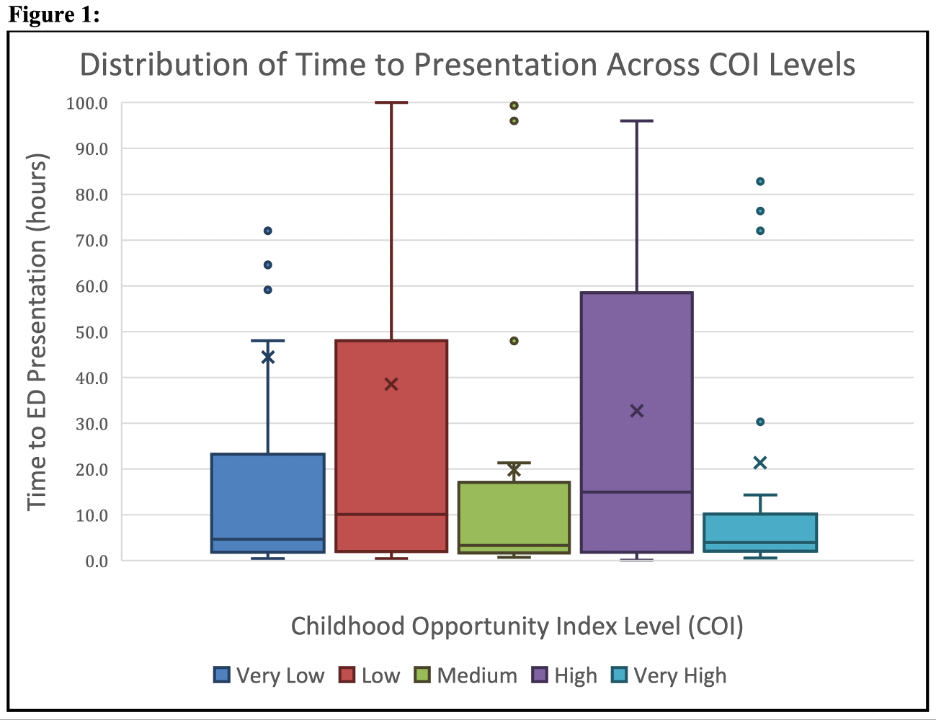
Design/Methods: This was a retrospective chart review of patients aged 29 days to 18 years assessed for stroke in a pediatric tertiary care center’s ED from January 2016 to December 2022. The COI 2.0 dataset was used to assign a COI score and quintile level to each patient based on their home zip code. Chi-square tests examined associations between demographic and clinical variables and TTP and DIT. ANOVA compared mean TTP differences across COI levels. Stepdown regression analysis identified variables independently associated with TTP or DIT. For TTP, binomial outcomes included: >4.5 hours (the tPA window of eligibility) and >24 hours (the thrombectomy window of eligibility). Delay in DIT was defined as >1 hour.
Results: There were 199 patients included in this study (mean age 10.7 years, 54% male, 52% public insurance). Median TTP was 5.7 hours (interquartile range 36.2 hours), and 44% presented in under 4.5 hours. There was no significant association between COI and TTP nor DIT. A history of seizures was independently predictive of presenting under 4.5 hours (p=0.014). English speakers were more likely to present under 24 hours (p=0.038). Normal speech and extremity strength were associated with DIT >1 hour, but these associations did not persist in multivariate analyses.
Conclusion(s): No association was found between COI and TTP nor DIT. This study’s limitations include its retrospective nature, single-center data, and small sample size. Patients with a history of seizures and English speakers may present to the ED earlier, possibly due to greater confidence in navigating the healthcare system. A prospective study could better explore factors causing delays in presentation in children experiencing strokes or stroke mimics.