Neonatology
Session: Neonatal General 3: Maternal and Fetal Medicine
79 - Evaluating the Relationship Between Maternal Vascular Reactivity Index at 24-30 Weeks Gestation and Neonatal Birth Outcomes
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 79
Publication Number: 79.564
Publication Number: 79.564

Rebecca Slotkowski, BS (she/her/hers)
Ph.D. Candidate
University of Nebraska Medical Center
Papillion, Nebraska, United States
Presenting Author(s)
Background: Hypertensive disorders of pregnancy (HDP) affect one in seven pregnancies in the US and can lead to adverse neonatal outcomes, including fetal growth restriction and preterm birth. Maternal endothelial dysfunction is implicated in the pathogenesis of HDP, and the vascular reactivity index (VRI) is a validated, non-invasive measure of endothelial function. However, it is unknown whether maternal VRI is associated with neonatal birth outcomes.
Objective: This study aimed to assess the relationship between maternal VRI between 24-30 weeks' gestation and neonatal birth outcomes (e.g. gestational age and birthweight).
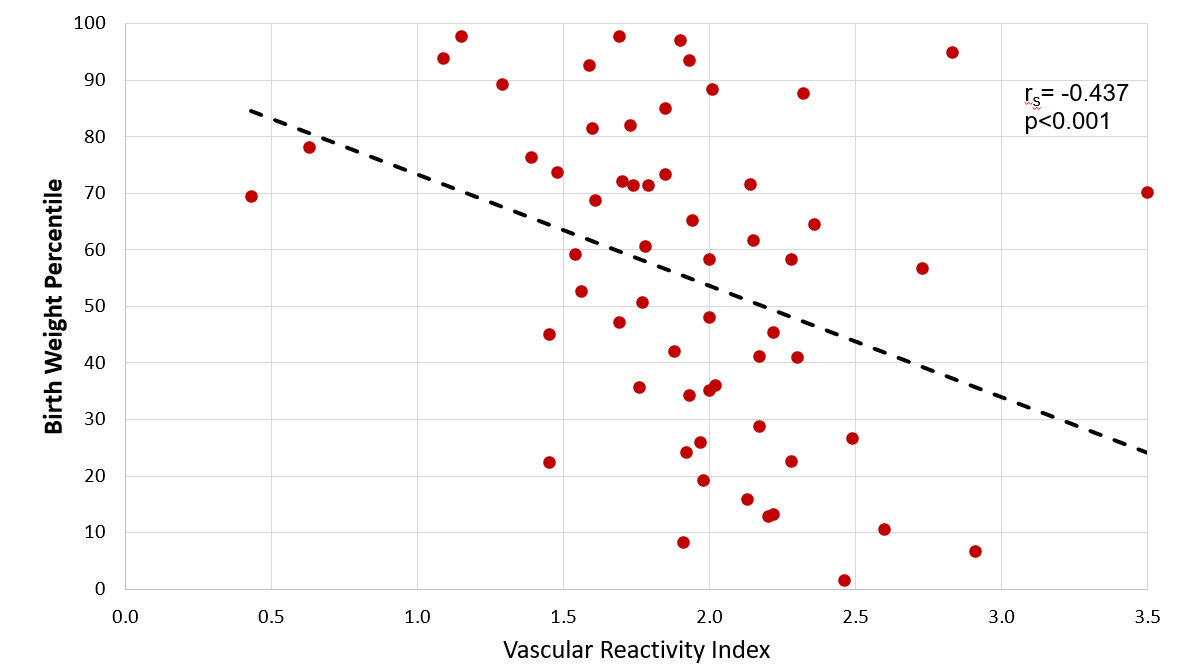
Design/Methods: An IRB-approved study enrolled 59 pregnant women who were receiving prenatal care at Nebraska Medicine (Omaha, NE, USA). VRI was measured between 24-30 weeks’ gestation using the Endothelix VENDYS machine per manufacturer protocol. In non-pregnant adult populations, a VRI below 1.4 is considered low reactivity, between 1.4-1.6 is average reactivity, and above 1.6 is high reactivity. Birth outcome data was collected from the electronic medical record. Spearman’s R assessed the relationship between continuous neonatal birth outcomes and VRI. A linear regression was performed to adjust for smoking, maternal age, and hypertensive status. A p-value < 0.05 was considered statistically significant.
Results: Median gestational age at birth was 39.3 weeks, with 50.8% female neonates and 49.2% male. Median maternal age was 32 years old and 42.4% of women had HDP. Median maternal VRI was 1.93 (IQR: 1.69-2.20). Gestational VRI was found to be inversely correlated with birthweight percentile (rs= -0.437, p< 0.001). After adjustment, a 1 unit increase in VRI predicted a 18.92% decrease in birth weight percentile (95% CI -32.90 to -4.93; p=0.01). Birth head circumference percentile (rs= -0.024, p=0.86), birth length percentile (rs= -0.080, p=0.55), and gestational age (rs= -0.227, p=0.08) were not significantly correlated with maternal VRI.
Conclusion(s): To our knowledge, our study is the first to assess maternal VRI during pregnancy in relation to neonatal birth outcomes. Surprisingly, VRI appears to be inversely related to birthweight percentile. Further studies with larger sample sizes are needed to explore this trend.