Neonatology
Session: Neonatal Neurology 2: Clinical
20 - Distinguishing perinatal stroke from HIE in encephalopathic newborns that undergo therapeutic hypothermia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 20
Publication Number: 20.491
Publication Number: 20.491

Fernando F. Gonzalez, MD (he/him/his)
Professor
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Perinatal stroke is a common cause of full-term perinatal brain injury for which there are currently no specific therapies. A small proportion of babies with stroke present with encephalopathy that is consistent with HIE and therefore qualify for cooling. Diagnosis is not made until MRI is performed.
Objective: Determine differences in risk factors, presentation or hospital course that would enable early distinction between HIE and stroke.
Design/Methods: High-dose Erythropoietin for Asphyxia and Encephalopathy (HEAL) Trial participants who underwent MRI were included. Stroke was defined as focal ischemic infarct(s), typically wedge-shaped, within an arterial distribution (e.g., Middle Cerebral Artery). The primary outcome was death or neurodevelopment impairment (NDI) defined as cerebral palsy, Gross Motor Function Classification Score >=1 or cognitive score < 90 on Bayley III. Neurodevelopment was also categorized into a 5-level ordinal measure: none, mild, moderate, severe, or death for secondary analysis. We used generalized linear regression models to assess the relative risk of death or NDI by presence of stroke controlling for HIE severity.
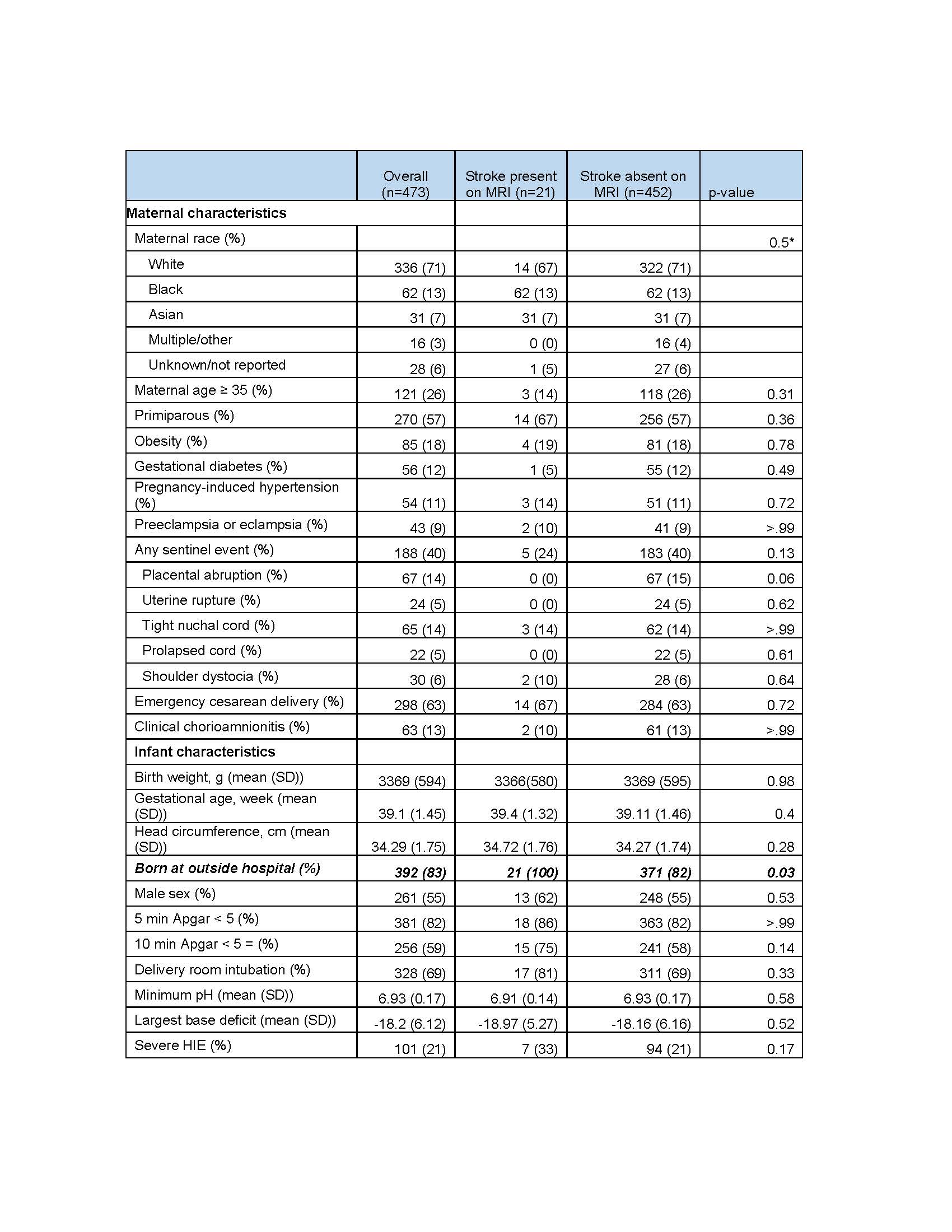
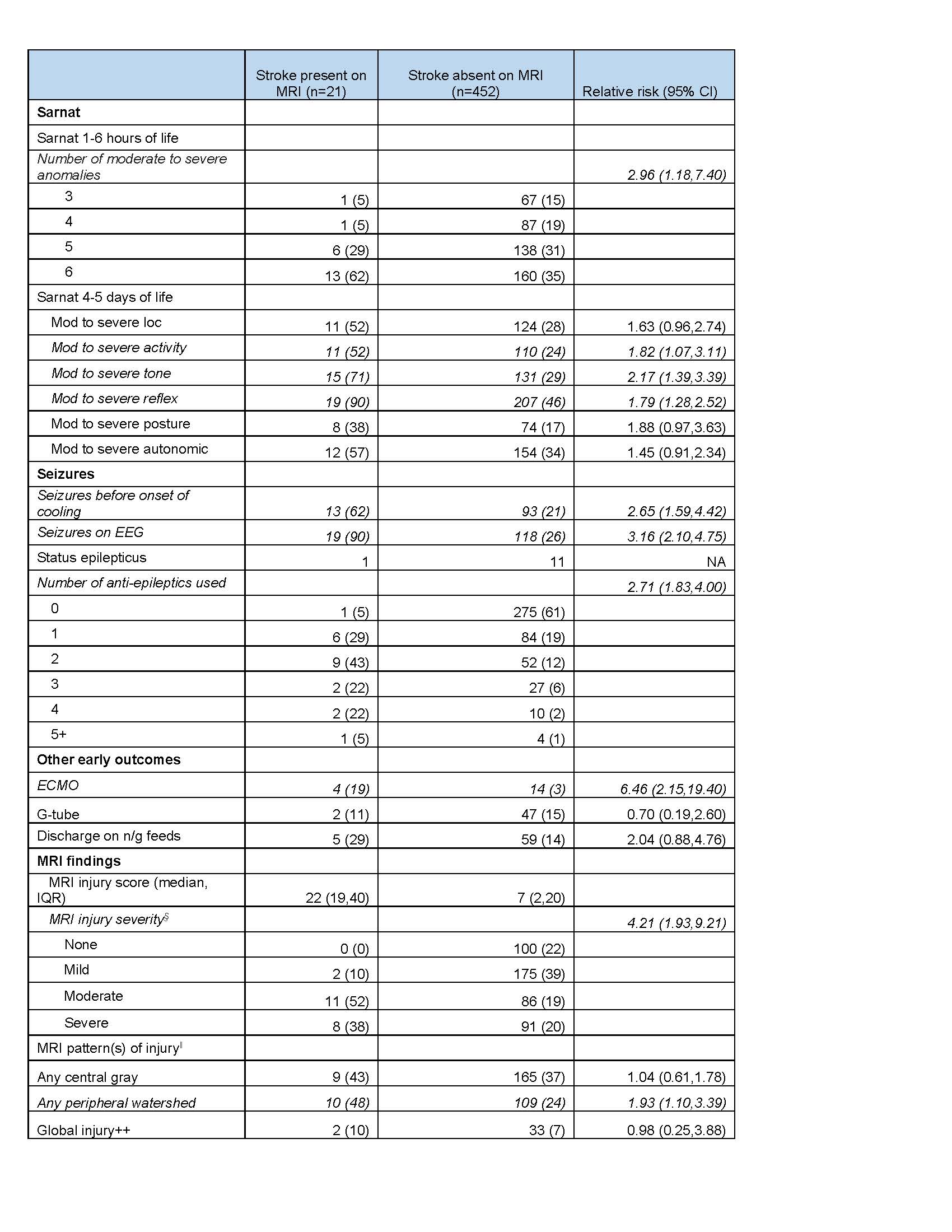
Results: Among 473 neonates with encephalopathy, 21(4%) had evidence of stroke and 13/21 subjects (62% of stroke) had evidence of stroke and HIE on MRI. Neonates with stroke were more likely to have been born at a referring hospital [n=21 (100%) for stroke vs. n=371 (82%) stroke absent, p=0.03; Table 1]. Subjects with stroke were more likely to have moderate or severe postural abnormalities (18/21, 86% vs. 256/452, 59%; RR1.37, CI 1.01,1.85), and had more moderate/severe abnormalities on Sarnat exam between 1 and 6 hours of life (RR 2.96, CI 1.18,7.40). Subjects with stroke were also more likely to have seizures before initiating cooling (13/21, 62% vs. 93/452, 21%; RR 2.65, CI 1.59,4.42), to receive anti-seizure medications (RR 2.71, CI 1.83,4.00), to receive ECMO (4/21, 19% vs. 14/452 (3%); RR 6.46, CI 2.15,19.40), and have more anomalies on day 5 Sarnat exam compared to subjects with no ischemic infarct (Table 2). There was no difference in primary or secondary outcomes among neonates with and without stroke (Table 3).
Conclusion(s): Cooled subjects with an ischemic infarct were more likely to have seizures, worse Sarnat exams, and receive ECMO. Among infants with encephalopathy, the presence of an ischemic infarct on MRI was not associated with 2-year outcomes. The majority of these subjects had MRI findings consistent with both stroke and HIE and may represent a sicker population.
.jpg)
