Neonatology
Session: Neonatal General 5: PDA, Surgical Conditions, Infections
139 - Single center retrospective review of IVIG use and associated morbidity and mortality in infants born at less than 28 weeks gestational age
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 139
Publication Number: 139.2253
Publication Number: 139.2253
- BO
Brittany O'Brien, DO (she/her/hers)
Pediatric Resident
University of Iowa Stead Family Children's Hospital
Coralville, Iowa, United States
Presenting Author(s)
Background: Intravenous immune globulins (IVIG) have been used to treat children since 1952. Though IVIG use has increased for various indications, the majority are off label. Common indications for IVIG include hemolytic disease of the newborn, necrotizing enterocolitis (NEC), sepsis, and immunoglobulin deficiency. The recent 2022 AAP guidelines on hyperbilirubinemia of the newborn warns about the potential of NEC and hemolytic anemia associated with IVIG.
Objective: Our objective was to compare the rates of NEC and number of red blood cell (RBC) transfusions in premature neonates that received IVIG treatment compared to those who did not.
Design/Methods: This was a single-center, retrospective review study of neonates who were ≤28 weeks gestational age (GA) and admitted to the neonatal intensive care unit (NICU) between Jan 2013 – July 2022. Our unit protocol includes screening all infants < 26 weeks GA or birth weight < 1000 grams with weekly IGG levels. If the level is < 200, patients receive IVIG to prevent nosocomial infections. IVIG is also given for sepsis, capillary leak syndrome, or hemolytic anemia.
We used database extraction for both maternal and neonatal demographic factors. Manual chart review was performed to review NICU morbidities, mortality, and specific laboratory values of interest. Maximum vasoactive-inotropic score (VISmax) was calculated for all patients to quantify the severity of critical illness to be compared between cohorts. T-test or chi squared was used for continuous and categorical variables, respectively. A multi-variable logistic regression with survival as the dependent variable was performed.
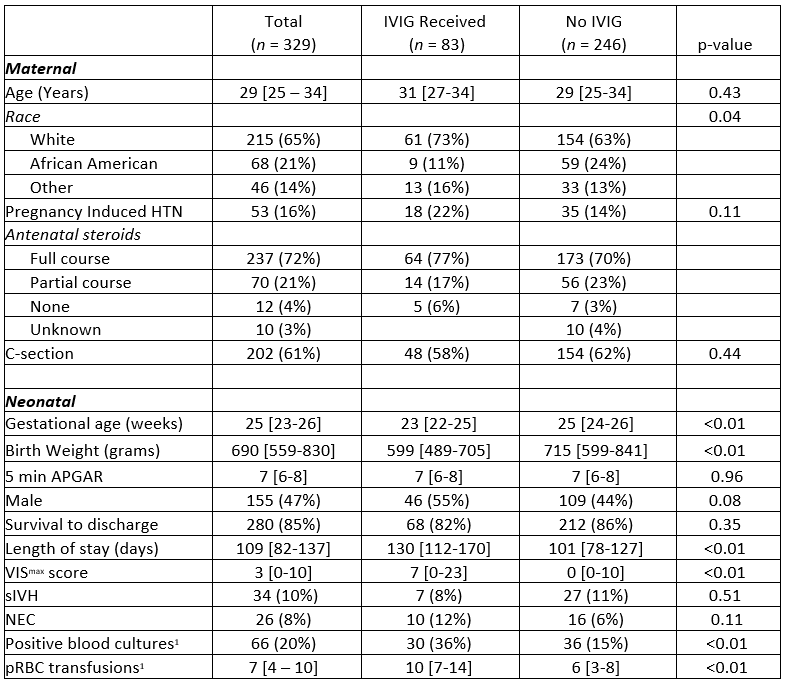
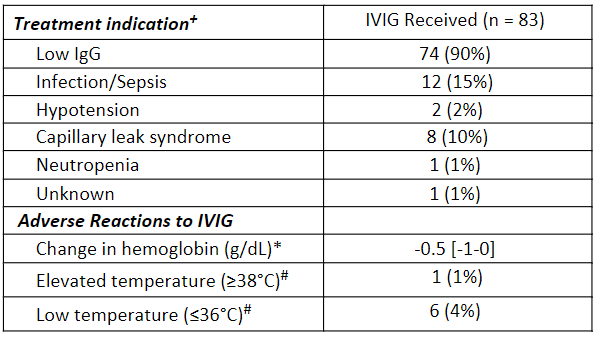
Results: 329 inborn infants met inclusion criteria. 83 received IVIG during hospitalization. The IVIG group received a median of 2 doses [IQR 1-2]. Table 1 shows the IVIG group had a significantly lower GA, birthweight, and higher VISmax. Length of stay, positive blood cultures, and RBC transfusions were found to be higher in the IVIG group, however, there was no difference in survival at discharge. There were multiple indications for IVIG and low incidence of adverse reactions (Table 2). Table 3 shows that receiving IVIG and a lower VISmax were significantly associated with survival.
Conclusion(s): The lack of mortality difference between these two groups despite a difference in clinical disease severity suggests that IVIG may provide a clinical benefit to the sickest patients. The increased number of RBC transfusions and positive blood cultures in the IVIG group is likely due to the sentinel event that preceded IVIG administration, but this temporal relationship requires further analysis.
.png)
