Neonatology
Session: Neonatology Pulmonology Clinical Science 1: Bronchopulmonary Dysplasia
568 - The association between bronchopulmonary dysplasia severity and its risk factors and long-term outcomes: comparison of three definitions
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 568
Publication Number: 568.1546
Publication Number: 568.1546

Trix A. Katz
PhD student - Pediatric Resident
Emma Children's Hospital, Amsterdam University Centers
Amsterdam, Noord-Holland, Netherlands
Presenting Author(s)
Background: The validity of the current bronchopulmonary dysplasia (BPD) definitions in preterm infants is under debate. The 2001-National Institute of Health (NIH), the 2018-NIH and the 2019-Jensen bronchopulmonary dysplasia (BPD) definitions classify infants in three grades of BPD severity. It is not clear which definition performs best in ordinal prediction of long-term outcome and the presence of BPD risk factors.
Objective: To compare the association of the severity categories of these BPD definitions with neurodevelopmental and respiratory outcomes at two- and five years corrected age (CA), and several BPD risk factors such as gestational age (GA), birthweight (BW), small for GA, total days of supplemental oxygen- and invasive mechanical ventilation (IMV).
Design/Methods: In this retrospective cohort study, outcomes of infants born between 2009 and 2015 at the Amsterdam University Medical Centers with a gestational age < 30 weeks were collected. The primary outcomes were neurodevelopmental impairment (NDI) or late death, and respiratory morbidity at two- and five-years CA. Using a Firth’s logistic regression and Brier scores, we investigated if the ordinal grade severity is associated with incremental increase of adverse long-term outcomes.
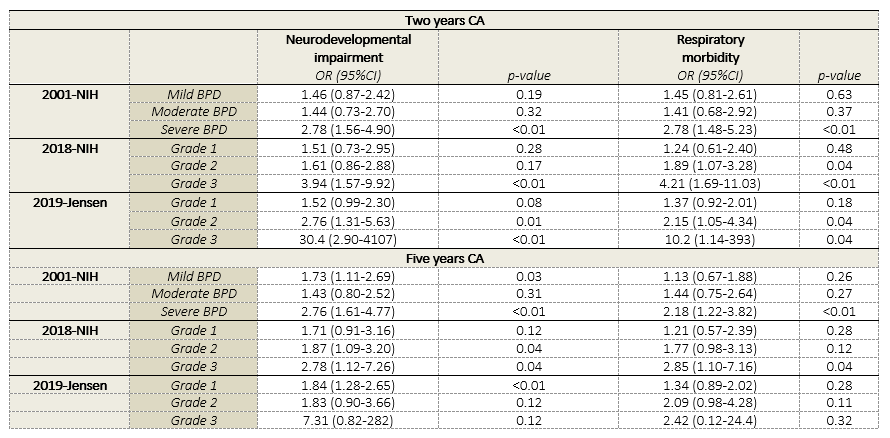
Results: 584 preterm infants (median GA 28.1 weeks and BW 1040 g) were included and classified according to the three BPD definitions. In general, none of the definitions showed a clear ordinal incremental increase of risk for any of the outcomes with increasing severity classification (Table 1). No significant differences were found between the three BPD definitions (Brier scores 0.169 to 0.230, Table 2). However, the Brier scores for all three BPD definitions are classified as non-informative and ill-calibrating. Respiratory interventions, but not GA, birth weight or small for GA, showed an ordinal relationship with BPD severity in all three BPD definitions.
Conclusion(s): The severity classification of three BPD definitions showed low accuracy of the probability forecast on NDI or late death and respiratory morbidity at two- and five-years CA, with no differences between the definitions. We found that only the most severe forms of BPD have a significant increased risk of poor outcome. If deemed important to clinicians and researchers for BPD to be an ordinal severity-based definition, future initiatives need to be focusing on the calibration as well as the discriminative predictive performance of BPD definitions.
.png)
