Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 3: Enteral Nutrition
437 - The Impact of Opt-in versus Opt-out Consent Model on Mother’s Own Milk and Feeding Practice in Preterm Infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 437
Publication Number: 437.1884
Publication Number: 437.1884

Christhian A. Cano-Guerra, MD (he/him/his)
Resident Physician
Tufts Medicine Pediatrics
Boston, Massachusetts, United States
Presenting Author(s)
Background: A mother’s own milk (MOM) is the optimal nutrition source. However, when MOM is not available or insufficient, pasteurized donor human milk (PDHM) is a safe alternative, especially for very low birth weight (VLBW) infants. To expedite the availability of PDHM, in November 2018, our NICU switched from the traditional opt-in consent to an opt-out consent model.
Objective: To evaluate feeding practice, growth trajectory, and the rate of MOM usage in VLBW infants before and after implementing the opt-out consent model.
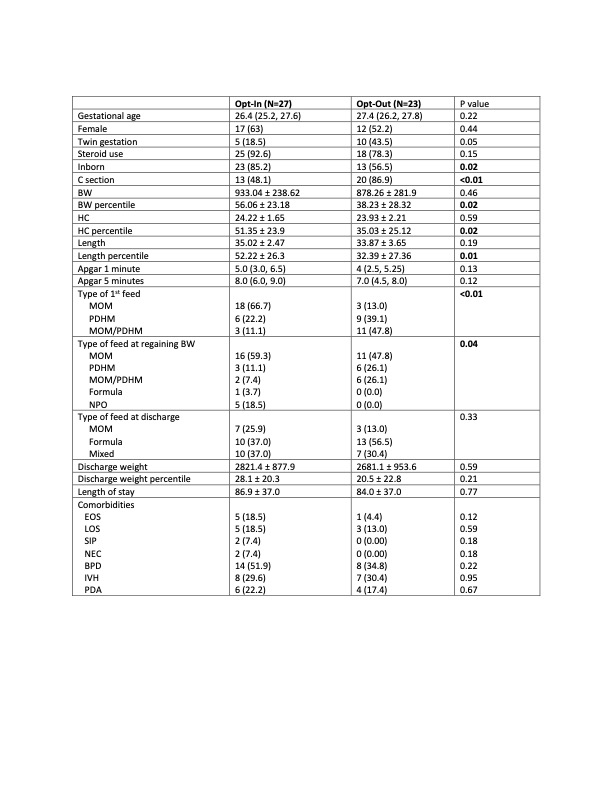
Design/Methods: A retrospective chart review was conducted in neonates ≤ 28 weeks gestational age (GA) born between November 2016 and December 2022. Subjects were divided into two epochs: opt-in (November 2016-October 2018) and opt-out (January 2019-December 2022). Neonatal data collected included GA, sex, steroid use, birth location, delivery method, anthropometric measures, feeding/growth information. Central line duration and comorbidities, e.g., SIP, BPD, IVH, were also included. Comparisons were made between the two consent models. Continuous variables were analyzed using a student’s t-test and categorical variables using a Chi-squared test.
Results: Fifty neonates were included in the current analysis (Table). There were significantly fewer inborn and more C-section deliveries in the opt-out cohort. In the opt-out model, enteral feed was initiated significantly earlier, and neonates tend to reach full feed and regain birth weight faster than those in the opt-in model. Although not significant, the central line duration was shorter in the opt-out model (Fig. a). While the opt-out cohort was significantly smaller at birth, over time their growth was comparable with the opt-in cohort (Fig. b). There was a significant difference in the type of milk used at first feed and the time to regain BW, however, this difference was not sustained at discharge. No significant difference was seen in the comorbidities (Table).
Conclusion(s): The opt-out consent model for VLBW infants at our center was associated with a significant reduction in the time to first feed and other benefits, e.g., decreased central line duration, faster time to reach full feed and regain BW, albeit no significant effects on comorbidities. The opt-out model did not affect the rate of MOM usage. The growth trajectory was comparable, irrespective of the consent models. While limited by the retrospective nature of this study, our pilot data provided evidence of potential benefits related to the opt-out consent model. Future analysis will use a larger sample size.
.png)
