Neonatology
Session: Neonatal General 4: Nutrition, Feeding, and Growth
95 - Diverse Enteral Feeding Practices in Contemporary ELBW Infants in the Connection Trial
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 95
Publication Number: 95.235
Publication Number: 95.235

Scott O. Guthrie, MD
Professor
Vanderbilt University School of Medicine
Jackson, Tennessee, United States
Presenting Author(s)
Background: Enteral feeding is key to the development of premature infants.
Objective: Investigate enteral feeding practices among high-level NICUs recruiting more than 20 ELBW infants each into the ‘Connection Trial’ (ClinicalTrials.gov ID: NCT03978000).
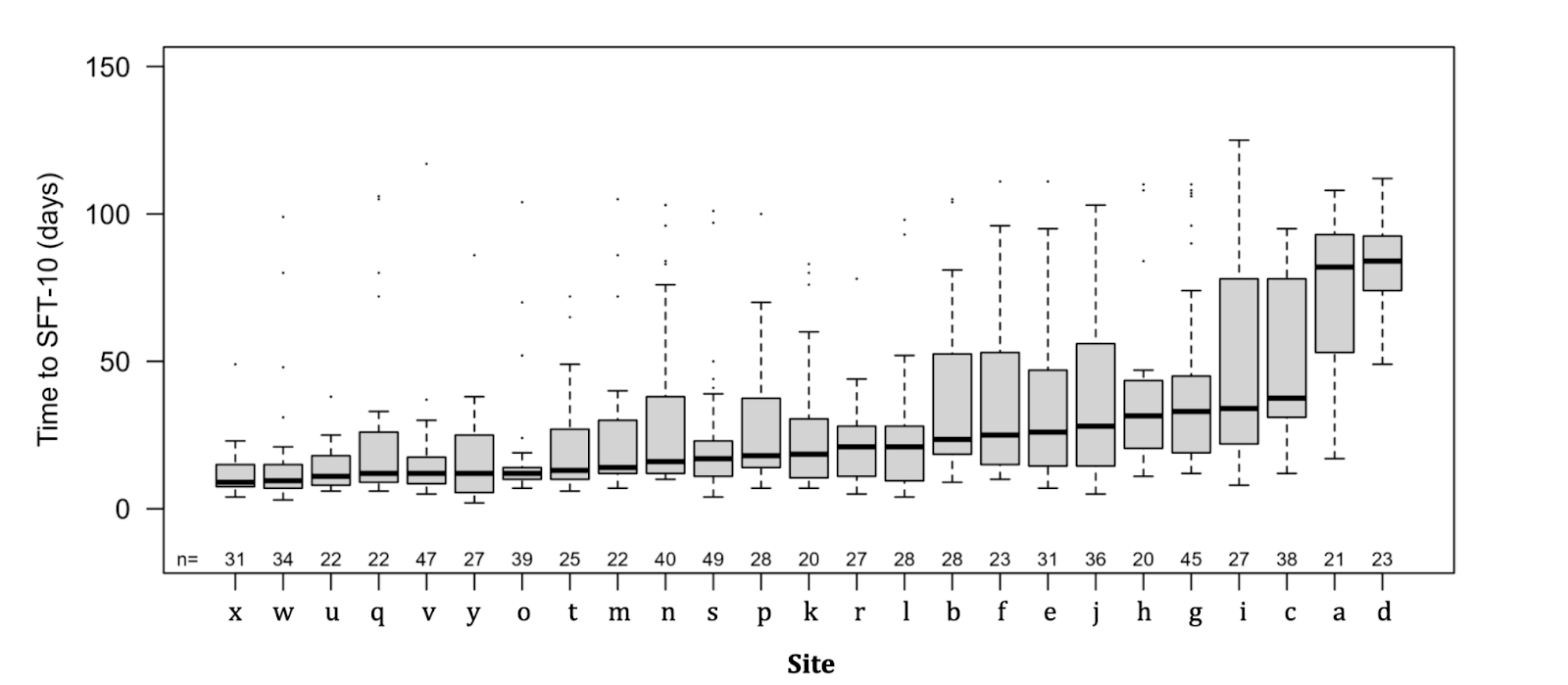
Design/Methods: 25 units enrolled up to 49 ELBW infants (total 753 infants) with median BW and GA at birth ranging from 750g to 930g and 25w to 28w, respectively. The ‘Connection Trial’ is phase 3 registration trial conducted under US IND and EU CTX. It compares the potential new biological entity IBP-9414 (L. reuteri) vs placebo with time to sustained feeding tolerance (SFT) as a primary endpoint. SFT is defined as >10 consecutive days with the combined requirement of the infant receiving enteral feeds totalling >120 mL/kg/day with no parenteral nutrition and growing at mean >10g/kg/day. Daily recording of enteral feeding volumes, any use of mother’s milk and parenteral nutrition as well as adverse events (AE) and serious AE (e.g. life-threatening) were gathered and merged into median values per unit during the median 56 study days (IQR 46-66 days).
Results: Kaplan-Meier estimates of total enteral feeding volumes showed that >10mL/kg/day was reached at median 2 to 11 days and the more composite endpoint of SFT at median 9 to 84 days of age (Fig. 1). Any mother’s milk was given during median 95% (IQR 85-100%, range 0-100%) and parenteral nutrition during 33% (IQR18-60%, range 0-100%) of the study days. Median duration of intravenous antibiotics use was 8 days (IQR 2-18 days). Median feeding volumes at postnatal day 5 correlated strongly with those at day 15 (r=0.67, p=0.0002). Units increasing enteral feeding volumes faster, in comparison to those progressing the volumes slower, reached SFT earlier (Fig. 2) and used less intravenous antibiotics despite culture-positive late onset sepsis being similarly common, used mother’s milk more frequently and less parenteral nutrition, and reported more frequent signs of feeding intolerance. The differences in median feeding volumes did not seem to depend on differences in BW and GA at birth nor on the incidences of infant morbidities as any SAE, GI SAEs like NEC, perforation and obstruction, GA AEs and extra-GI SAEs.
Conclusion(s): Early enteral feeding practices varied across the units and seemed to rely on factors other than birth characteristics and morbidities in the investigated, contemporary ELBW infants.
.png)