Immunizations/Delivery
Session: Immunizations/Delivery 1
34 - Uptake of Recommended Adolescent Vaccines Among U.S. Military Dependents During the COVID-19 Pandemic
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 34
Publication Number: 34.1515
Publication Number: 34.1515

Jessica Wilder, MD (she/her/hers)
Pediatrics Resident
Naval Medical Center Portsmouth
Virginia Beach, Virginia, United States
Presenting Author(s)
Background: The COVID-19 pandemic had far-reaching impacts on the delivery of preventive healthcare to pediatric patients worldwide. The disruption in “well-child” visits and a rise in vaccine hesitancy has affected the U.S. Military Health System (MHS) as well. We aimed to measure the delivery of 3 vaccines (Neisseria meningitidis serogroup B (MenB), influenza virus, and COVID-19) that are recommended to adolescent patients, but not required by any U.S. states for K-12 school attendance.
Objective: Our goal was to compare uptake of these vaccines among specific populations over the course of the pandemic to detect existing disparities and identify groups that would benefit most from targeted vaccination initiatives.
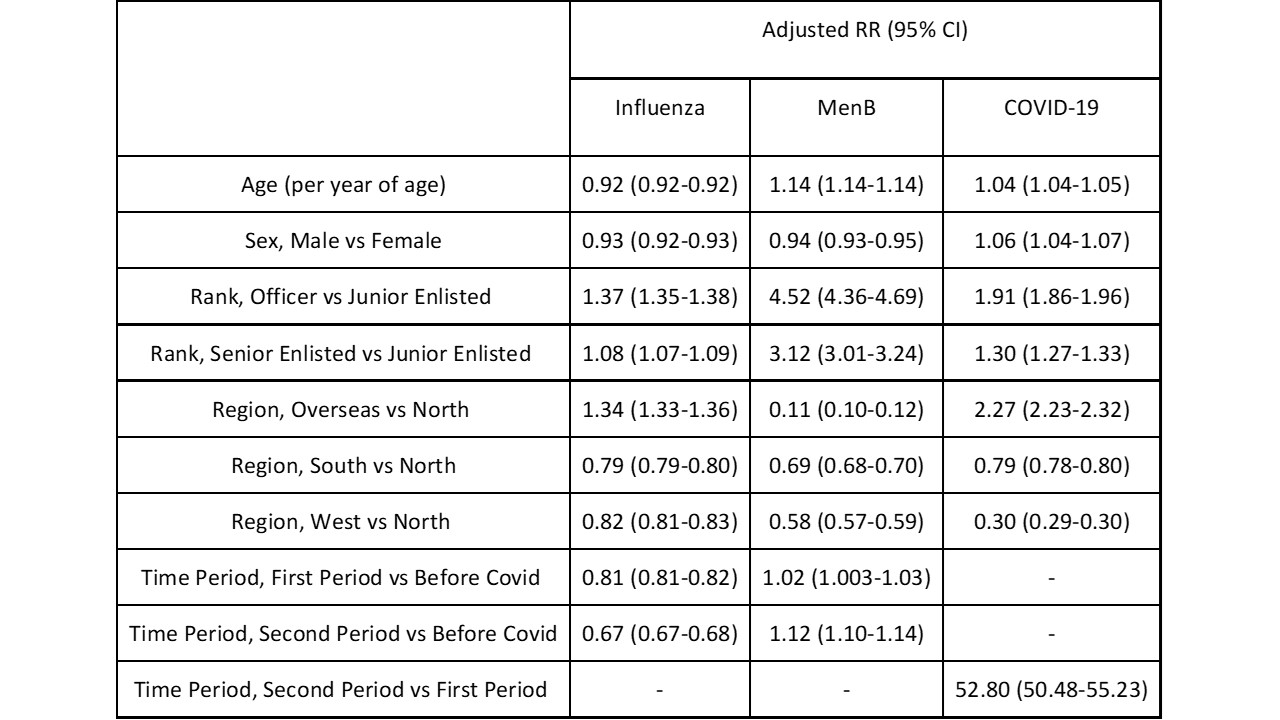
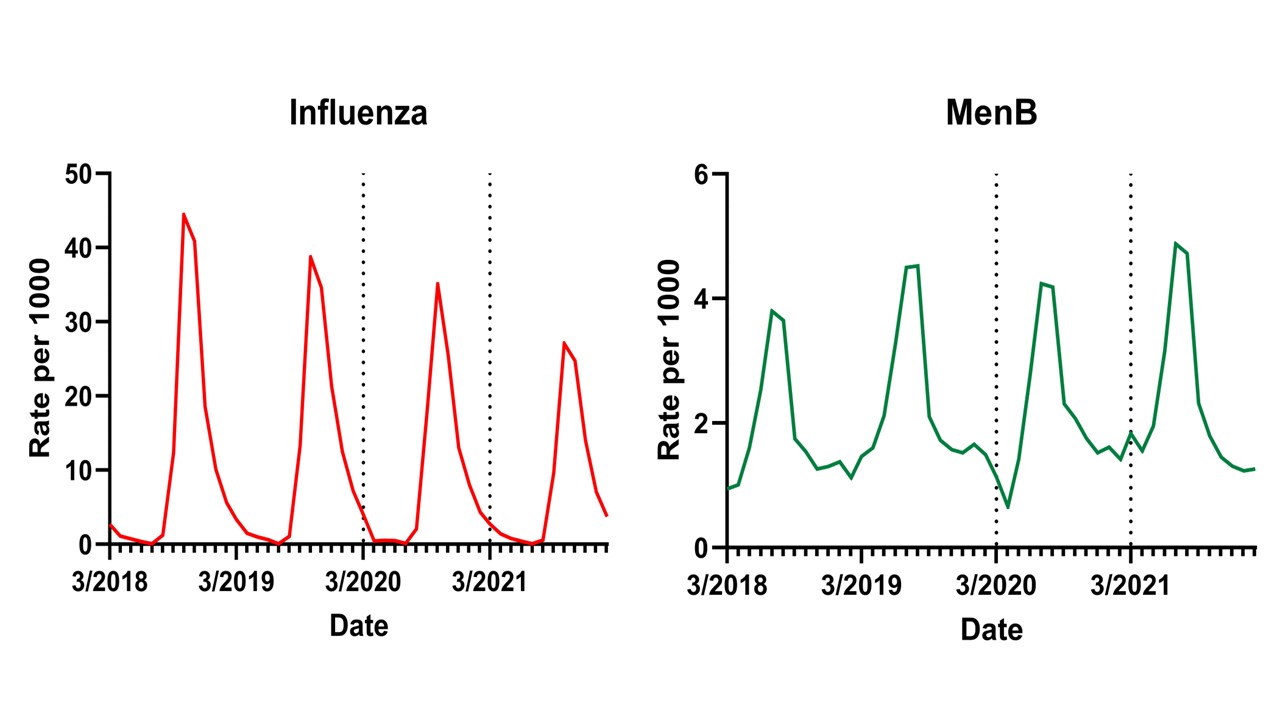
Design/Methods: We performed a retrospective repeated monthly cross-sectional study using data from TRICARE Management Activity’s MHS Database. We included dependents aged 11-21 years who were eligible for MenB, influenza, and COVID-19 vaccines from January 2019 to August 2023. We indirectly measured vaccine uptake by dividing the number of Current Procedural Terminology-coded vaccinations administered per month by the number of total patients eligible in that same month to calculate rate ratios. We then used adjusted Poisson regression to compare rate ratios for each vaccine by age, sex, sponsor rank, and geographic region.
Results: Median monthly vaccination rates for influenza among adolescents were 19% and 33% lower respectively in the first and second year of the COVID pandemic compared to pre-pandemic years. Rates of MenB vaccination were 18% higher in the COVID pandemic period than years prior. For the months when COVID-19 vaccines were available, adolescents living outside the continental U.S. had >2-fold higher COVID-19 vaccination rates than those living in the U.S. For all three vaccines, adolescent children of officers had considerably higher rates of vaccine uptake than those of lower-ranking enlisted members.
Conclusion(s): Although adolescents in the U.S. MHS have universal access to healthcare, influenza vaccination rates have fallen significantly in the COVID pandemic years. Rates of MenB vaccination, however, rose significantly in this same time period, possibly due to increasing requirements for this vaccine in higher education. The large differences in vaccination rates between children of officers and enlisted servicemembers is noteworthy, as lower military rank generally denotes lower socioeconomic status and educational attainment. Our data highlight potential education gaps and disparities in this population that must be addressed.
.jpg)
