Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
34 - Improving Passive Smoke Exposure Screening for Hospitalized Children
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 34
Publication Number: 34.3176
Publication Number: 34.3176

Rachel N. Vercillo (she/her/hers)
Medical Student
SUNY Upstate Medical University
Syracuse, New York, United States
Presenting Author(s)
Background: Hospitalized children are more likely to have passive smoke exposure (PSE), as studies have shown PSE to be an independent predictor of poor health outcomes in pediatric patients. Adult smoking rates in our area (18.5%) are higher than the national average (13.5%). A child’s hospitalization can be an opportunity to address, counsel and provide resources for parental smoking cessation. But PSE was infrequently documented (30%) and therefore was rarely addressed during hospitalization.
Objective: This is the first phase in a multiphase effort to screen all pediatric inpatients for PSE and to provide counseling and resources to the smoking parent. The first phase of the study was to improve PSE screening among nurses and residents to 50%. We also looked for trends in PSE screening rates among different chief complaints and demographic subgroups.
Design/Methods: Interventions for nurses included a 15-minute education session and signs at nursing stations encouraging PSE documentation during patient intake. Nurse managers reminded nurses to document PSE during nursing huddles for one week. Months later, nurse practitioners and residents were addressed at Grand Rounds and made aware of the project and the importance of documenting PSE as the first step for cessation counseling. Next, family facing signs were posted offering parents smoking cessation resources and counseling during their child’s stay. Finally, PSE was added to the required nursing intake form. Data was collected from the first ten consecutive pediatric patients admitted each week from 1/1/23-9/31/23. Chart review was performed to determine nursing and provider documentation, along with race, zip code, and admitting diagnosis.
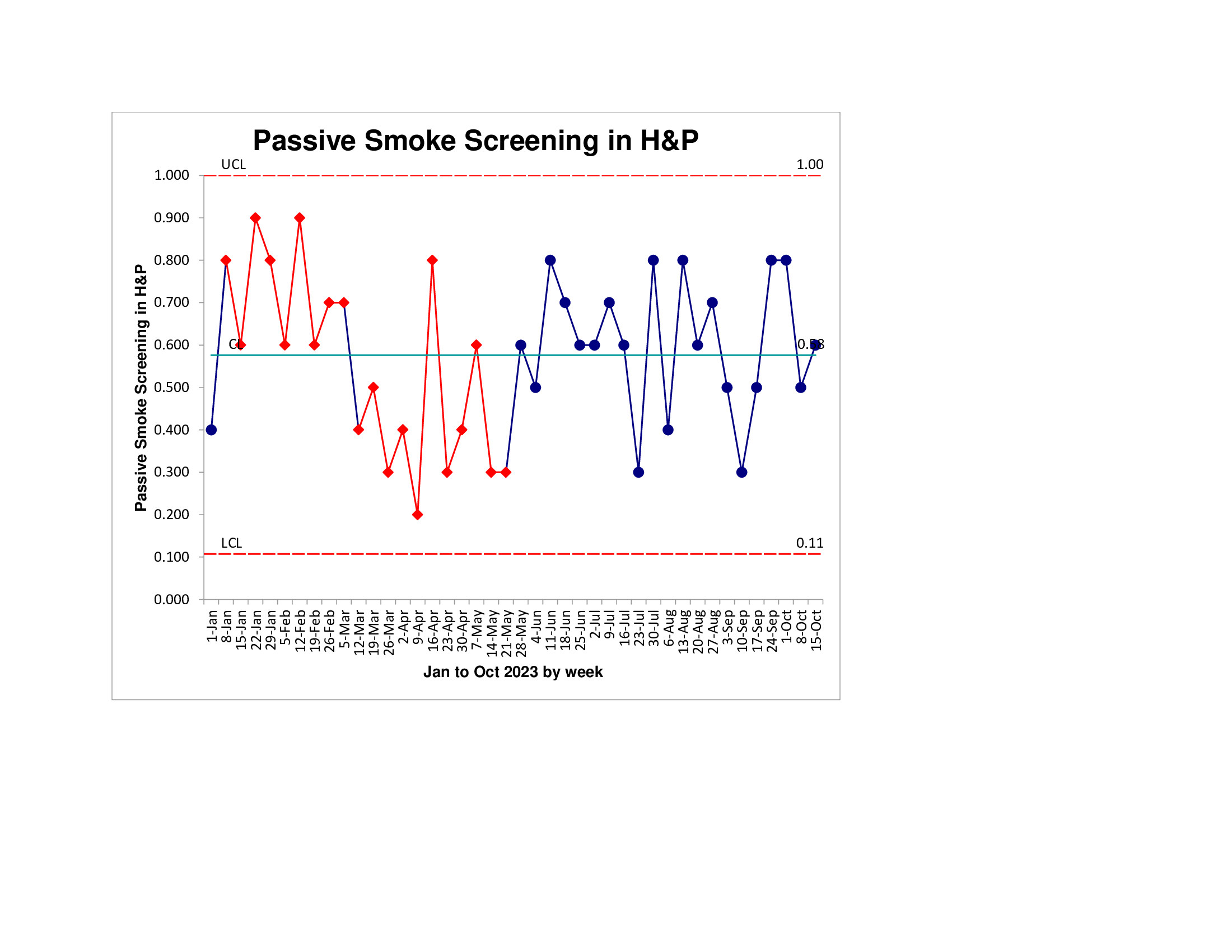
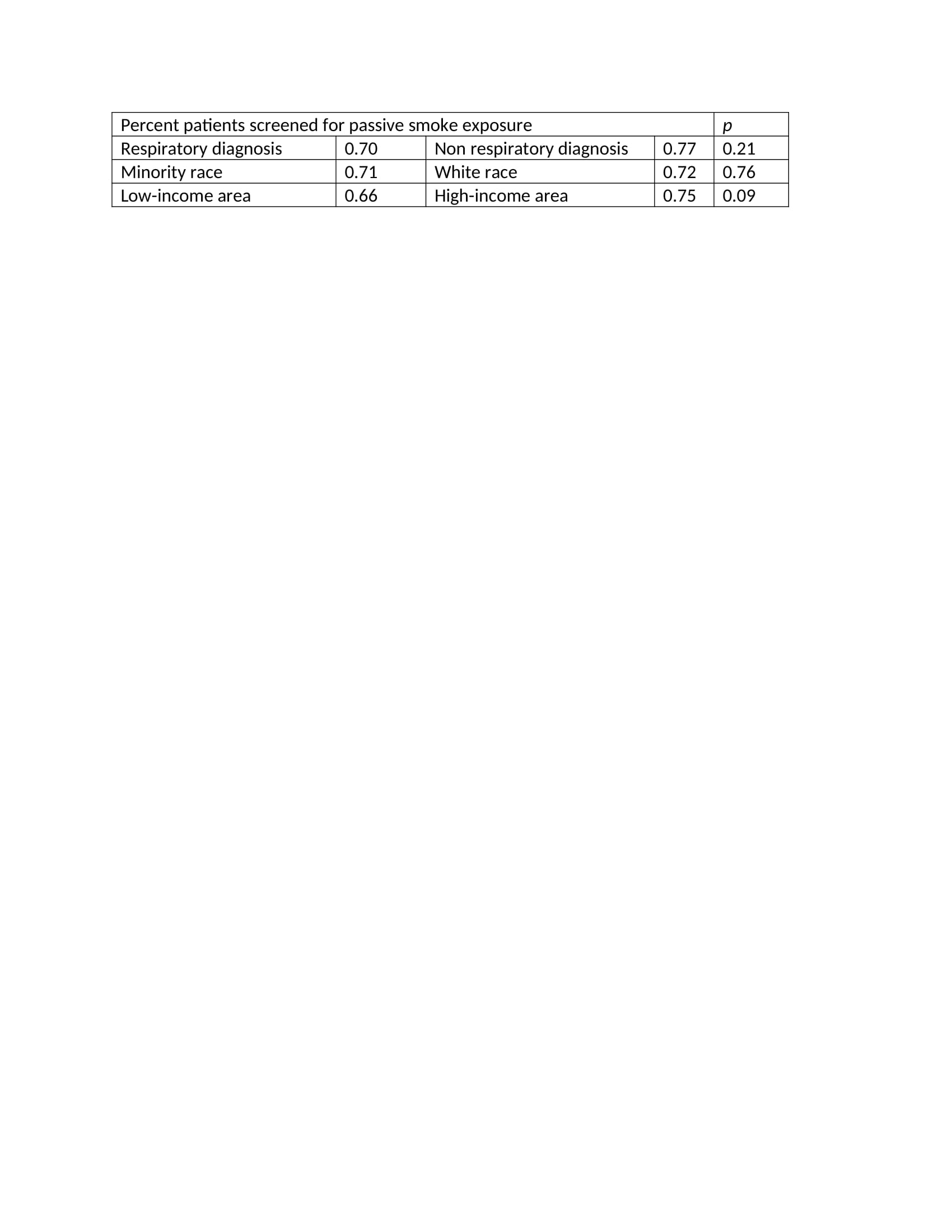
Results: Baseline screening rates were 32%. Nursing education had a sustained improvement on screening rates (Fig 1). There was rapid improvement following provider education to 80%, but this was not sustained. Overall, screening rates improved to a sustained 49% with statistical significance. Subgroup analysis by role showed no statistical improvement in physician documentation during the study period. We found no significant difference in screening rate based on diagnosis, minority race, or low income.
Conclusion(s): Improvement in screening for PSE was seen after cumulative interventions to address the importance of identifying passive smoke exposure from a nursing, physician, and family viewpoint. Screening for PSE did not differ based on the child’s race, admitting diagnosis, or income level. Further interventions are needed to address physician documentation of passive smoke exposure at our hospital.
Percent-Passive-Smoke-Nursing-.jpeg