Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 4: Congenital Heart Disease
170 - Reducing Adverse Delivery Outcomes Through Teleneonatology: A Randomized Simulation Trial
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 170
Publication Number: 170.3068
Publication Number: 170.3068

Samuel Gentle, MD
Assistant Professor
UAB
Birmingham, Alabama, United States
Presenting Author(s)
Background: With the reported decline in obstetrical services in many regions of the country, there is an increasing likelihood of an infant delivery at a hospital with a lower level of care. Teleneonatology, the use of telemedicine for newborn resuscitation and care, may bridge the resuscitation quality gap by connecting these hospitals with experienced care providers.
Objective: In a simulated neonatal resuscitation, we hypothesized that teleneonatal resuscitation, compared to usual resuscitation, would reduce the no flow fraction.
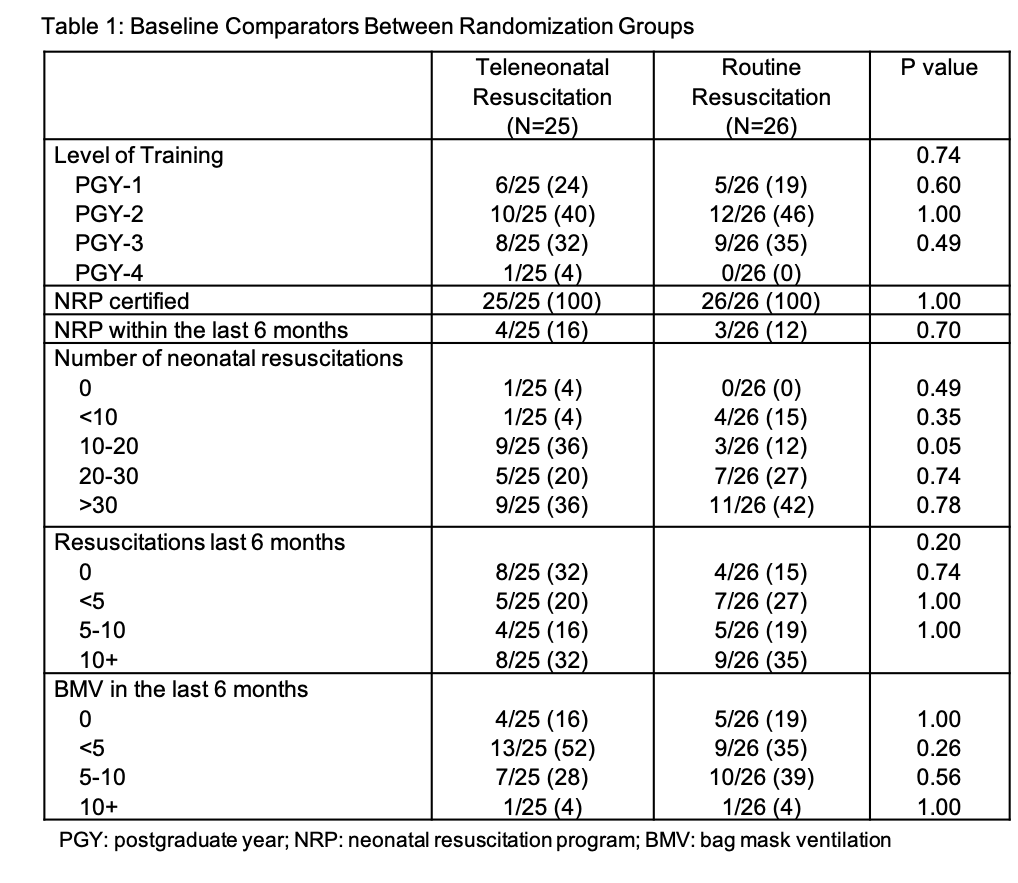
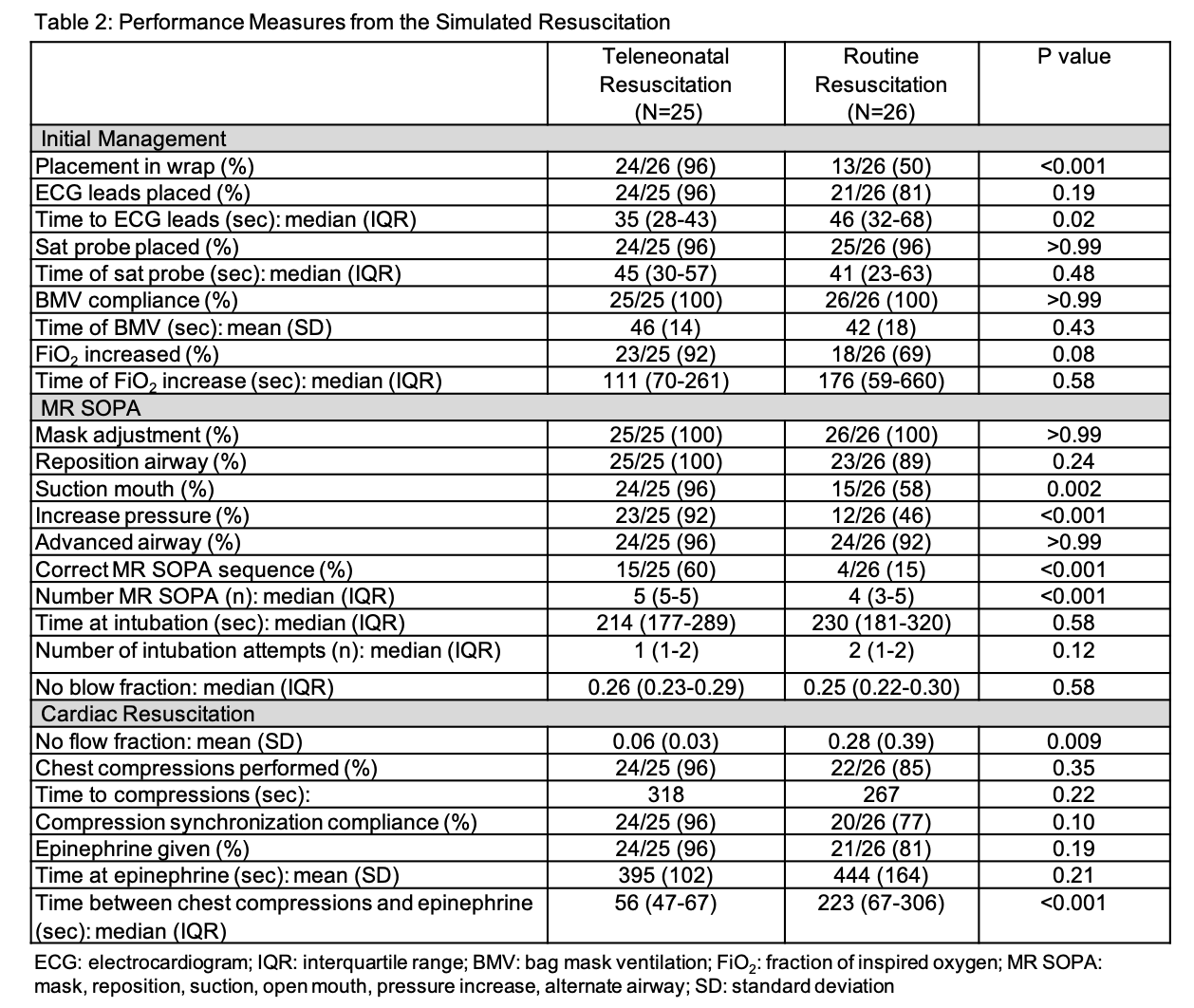
Design/Methods: This was a randomized simulation trial conducted at the University of Alabama at Birmingham between November 2020 and January 2023. Following informed consent, pediatric residents were randomized to either teleneonatal or routine resuscitation. Stratification was performed according to trainee level (PGY1 vs PGY2-4). For trainees randomized to teleneonatal resuscitation, a neonatologist joined remotely and facilitated resuscitation via an Amwell telemedicine cart. A Laerdal Premature Anne high fidelity manikin was used in the simulated scenario. In the scenario the manikin’s heart rate declined subsequent to intubation for which chest compressions and epinephrine administration were indicated. The primary outcome was no flow fraction defined as time without chest compressions divided by the time without spontaneous circulation when the heart rate was < 60. Secondary outcomes included binary outcomes of neonatal resuscitation including modifications of bag mask ventilation, and the use of chest compressions and epinephrine as well as time elapsed prior to these interventions. Assessments were made by investigators blinded to group allocation.
Results: One hundred fourteen trainees were approached during the study period of which 51 were consented and completed the scenario. There were no differences in baseline characteristics between randomization groups (Table 1). The no flow fraction in the teleneonatal resuscitation group was lower than the routine resuscitation group (0.06 vs 0.28; p=0.009). Participants in the teleneonatal resuscitation group also more frequently correctly performed modifications of bag mask ventilation (60% vs 15%; p< 0.001) with a comparable time to intubation (214s vs 230s; p=0.58) and epinephrine (395s vs 444s; p=0.21) between groups (Table 2).
Conclusion(s): In this randomized simulation trial of neonatal resuscitation, teleneonatal resuscitation resulted in a reduction of adverse delivery outcomes compared to usual care. Further evaluation of teleneonatal resuscitation’s impact within clinical settings are warranted.