Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
35 - Elevating Care: High-Fidelity Simulation Training for Caregivers of Children Requiring Long-Term Mechanical Ventilation (LTMV) – Quality Improvement Initiative
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 35
Publication Number: 35.3079
Publication Number: 35.3079
.jpg)
Amit Agarwal, MD (he/him/his)
Professor of Pediatrics
University of Arkansas for Medical Sciences College of Medicine
Little Rock, Arkansas, United States
Presenting Author(s)
Background: Around 4,000 U.S. children receive tracheostomy yearly. A tracheostomy can transform the lives of the child and the caregiver, but it often leads to costly hospital readmissions and caregiver burdens due to preventable complications. Currently, tracheostomy education at our hospital includes a combination of didactic instruction and bedside skills demonstration on a tracheostomy doll. This is helpful; however, it does not allow the caregiver a learning environment to practice techniques using realistic emergency scenarios and equipment.
Objective: We hypothesized that incorporating high fidelity simulation mannequin training to our current discharge preparedness curriculum would increase caregiver confidence in recognizing and managing emergencies that frequently arise among tracheostomy and ventilator-dependent children and secondarily reduce the ten-day readmission rates due to preventable tracheostomy related adverse events (TRAE)
Design/Methods: This project began in June 2023 and is ongoing. Eligible participants include designated caregivers of children with tracheostomies and requiring LTMV who are preparing for initial discharge from the hospital. The curriculum consists of printed handouts and instructional videos on tracheostomy care, cardiopulmonary resuscitation training, and hands-on skills training using tracheostomy dolls and the “teach back” methodology. This is newly followed by three high-fidelity simulations of tracheostomy and ventilator emergency scenarios: (a) airway obstruction, (b) accidental decannulation, and (c) leak in the circuit. A video-based debriefing focuses on identifying and closing performance gaps. Learners can repeat scenarios until competency is obtained. Last, caregivers complete a 48-hour stay “room in” at the hospital, independently caring for their child in preparation for discharge.
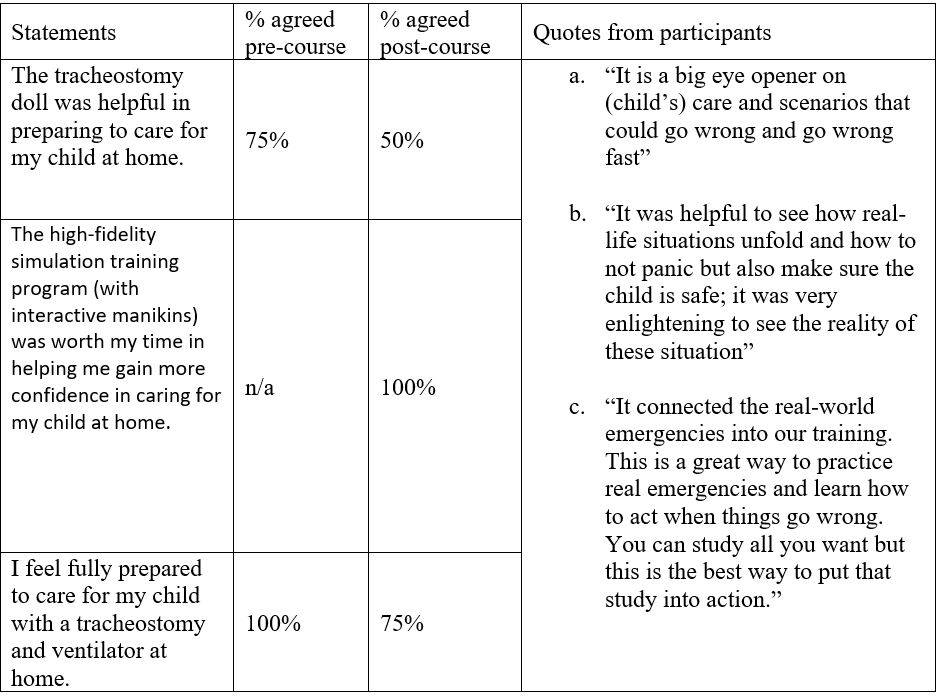
Results: Four family caregivers have completed the curriculum so far. The simulation-enhanced curriculum was well-received by participants. Participants reported that post-simulation debriefing was the most beneficial (Table 1). Interestingly, after going through the emergency scenarios, some parents asked for more practice using these simulations. The ten-day readmission rate due to preventable TRAE was 30% in the pre-implementation cohort (N=20) compared to 0% readmitted in the first ten days among the post-implementation cohort (N=4).
Conclusion(s): Preliminary data support the salutary effects of high-fidelity simulation on caregiver confidence. The use of quality improvement methodology is continuing to help improve the strength of this project during the development process.