Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 9
329 - Disparities in Pediatric Respiratory Illness Care in US Hospitals
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 329
Publication Number: 329.1828
Publication Number: 329.1828

Adria Bowles (she/her/hers)
Medical Student
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Respiratory illnesses are leading causes of childhood hospitalization, and disparities have been reported. Despite general/community hospitals providing most inpatient pediatric care in the US, care quality and disparities in these settings are poorly understood.
Objective: To evaluate disparities in respiratory illness care using a national sample of general/community hospitals.
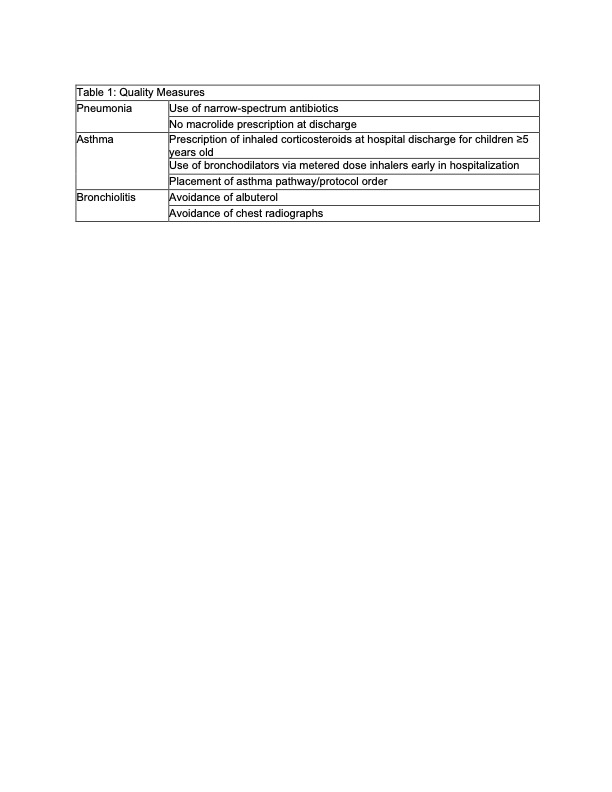
Design/Methods: SIP (Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children, NCT05206695) is a multicenter, randomized trial of a quality improvement intervention. This current study is a retrospective, observational study using pre-trial data collected via chart review at hospitals in the SIP trial. Patients were eligible if they had a primary diagnosis of asthma, pneumonia, or bronchiolitis and were admitted during 3 Winter seasons (2019-2022). We used multi-level regression models to evaluate care quality (Table 1) and health outcomes by race/ethnicity, payor (proxy for socioeconomic status), and primary language. Analyses of care quality only adjusted for age and sex. Analyses of health outcomes added predictors sequentially to assess potential contributions of each of these factors.
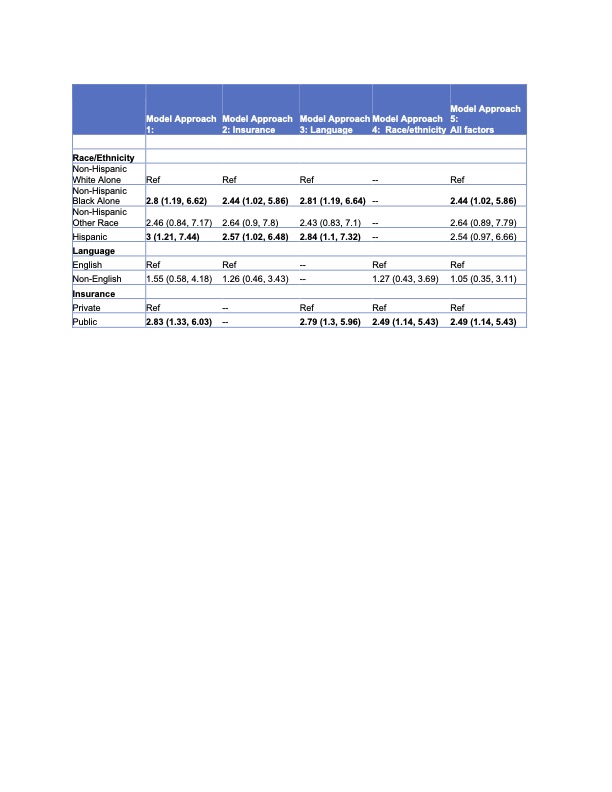
Results: We analyzed 2,390 admissions from 33 hospitals. Children with public insurance were more likely to receive recommended inhaled corticosteroids to control asthma (OR 1.72 [1.05, 2.81]) compared to those on private insurance, but there were no other differences in care quality. Hispanic and Non-Hispanic Black children with asthma were more likely to experience 30-day readmissions or ED revisits compared to Non-Hispanic White children (OR 3.00 [1.21, 7.44], OR 2.8 [1.19, 6.62], respectively) and these risks were significant even with adjustment for payor (Hispanic OR 2.57 [1.02, 6.48], Non-Hispanic Black OR 2.44 [1.02, 5.86]) or primary language (Hispanic OR 2.84 [1.1, 7.32]). Children with public insurance were also at greater risk compared to those on private insurance (OR 2.83 [1.33, 6.03]). We found no disparities in length of stay or ICU transfer.
Conclusion(s): In this national sample of general hospitals, we found public insurance may prompt greater prescription of preventive medications for asthma, but no other disparities in care quality. We found disparities in reutilization that persisted despite adjustment for payor and/or language, suggesting that structural racism plays a role in driving these disparities, independent of socioeconomic status or healthcare access. Addressing these disparities will require multifaceted, community-partnered interventions.
.jpg)