Health Services Research
Session: Health Services Research 1: Workforce
284 - Disruptive and Violent Behaviors at a Midwest Children’s Hospital
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 284
Publication Number: 284.1487
Publication Number: 284.1487
- AD
Adrienne DePorre, MD (she/her/hers)
Hospitalist
Children's Mercy Hospitals and Clinics
Childrens Mercy Kansas City
Prairie Village, Kansas, United States
Presenting Author(s)
Background: Workplace violence (WPV) in healthcare settings has become a priority of Occupational Safety and Health Administration, Joint Commission and Center for Medicare and Medicaid services. Despite the increasing ubiquity of violence within healthcare settings, the frequency and forms of violence are poorly described, particularly in pediatric care settings.
Objective: To describe patient care related violence within our dedicated pediatric health care system, including trends over time, persons involved, setting, and types of violent behaviors.
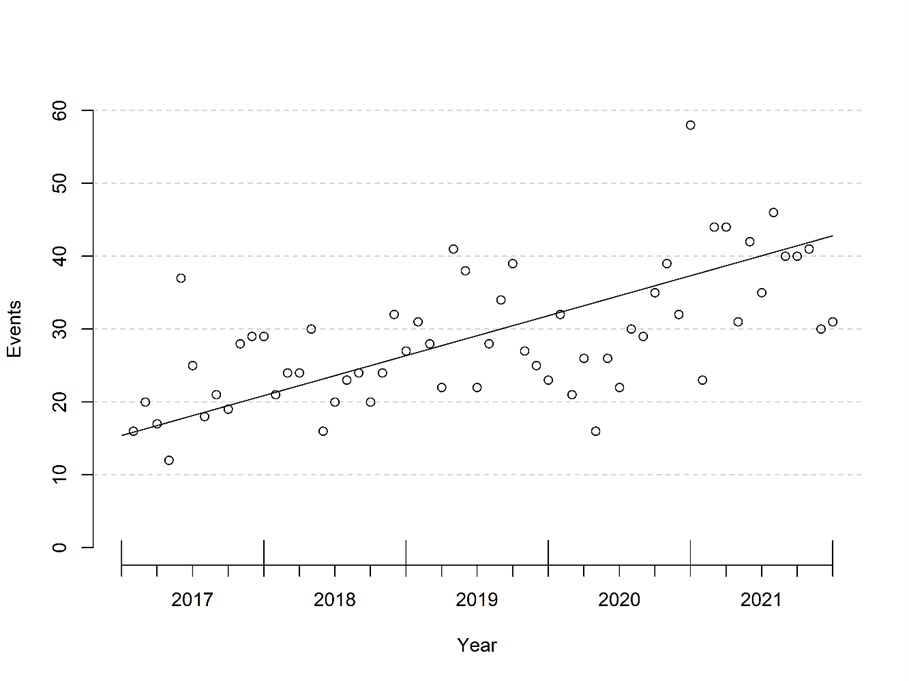
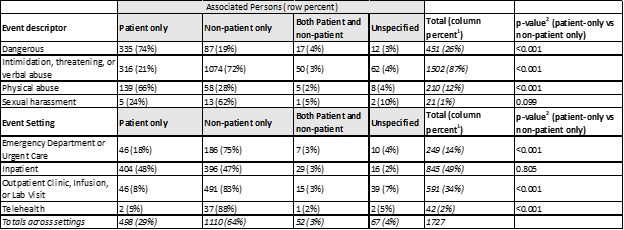
Design/Methods: We performed a review of disruptive events across our health system from 1/1/2015 to 12/31/2022 using our electronic health record. In our system, clinical staff may record events disruptive to patient care on a templated form, which includes person(s) engaging in the behavior(s),location, and a list of descriptors of behavior(s) witnessed. Using these descriptors, we analyzed violent events involving behavior described as “dangerous”; “intimidating, threatening, or verbal abuse”; “physical abuse”; and/or “sexual harassment”. To examine time trends, we plotted monthly violent event counts over time and used linear regression to model monthly event counts, each adjusted for the number of visits to our hospital that year, as a function of time.
Results: We identified 2201 violent events. In regression modeling, the trend for violent events increased over time ( Figure 1). Incidents increased by an average of 5.5 (95% confidence interval 4.2-6.7) per year (p < 0.001). The majority ( 64%) of all violent events were associated with non-patients; however among events with physical violence, the majority (66%) were associated with patients. Half (50%) of events occurred in the inpatient setting, 34% occurred in clinic, infusion, or lab settings, and 14% occurred in the Emergency or Urgent Care settings. Most (68%) events involved intimidation, threatening behavior, or verbal abuse, while 10% involved physical violence (Table 1).
Conclusion(s): WPV increased over time and most events were associated with non-patients. However, physical violence was most often associated with patients. While this is a single center study, our results emphasize the need for trauma-informed, proactive communication to both patients and visitors regarding behavioral expectations in ambulatory and inpatient settings, as well as transparent consequences for inappropriate behavior. Training staff on early recognition of patient/visitor agitation and techniques on de-escalation is critical to maintain workplace safety.