Adolescent Medicine
Session: Adolescent Medicine 1
140 - The Role of Family Support in Moderating Depression and Suicidality Amongst LGBTQ+ Adolescents in the Primary Care Setting
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 140
Publication Number: 140.247
Publication Number: 140.247

Joseph DelFerro, Jr., BS (he/him/his)
Medical Student
Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Lesbian, gay, bisexual, transgender, queer, and/or questioning (LGBTQ+) youth face worse mental health outcomes than their cisgender, heterosexual peers. Family support may mitigate this risk.
Objective: To compare depression and suicide risk between LGBTQ+ and non-LGBTQ+ youth in primary care and investigate effects of family support on mental health (MH) outcomes.
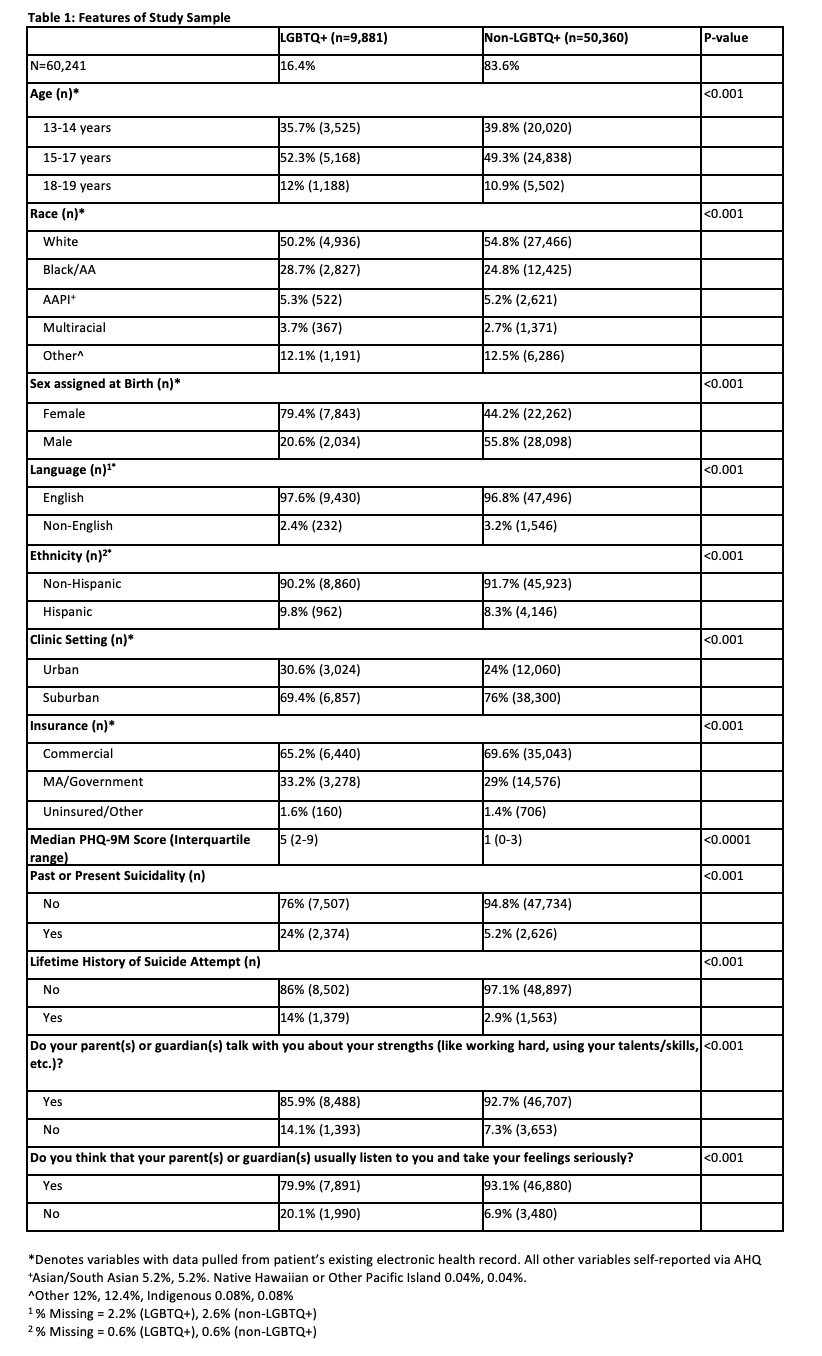
Design/Methods: This cross-sectional study used data from a 31-clinic primary care network from February 2022-May 2023. We included patients aged 13-19 who completed the Patient Health Questionnaire-9 Modified for Teens (PHQ-9M) and the Adolescent Health Questionnaire (AHQ)--an electronic screener that assesses LGBTQ+ identity, health behaviors, and parent/guardian (“parent”) support (discussion of teen strengths and listening to teens’ feelings). MH outcomes were 1) PHQ-9M score and 2) past and/or present suicidal ideation. Chi-square and Wilcoxon rank sum tests assessed associations between LGBTQ+ status and MH outcomes. Adjusted regression models assessed relationships between LGBTQ+ status and each MH outcome, with separate models including each support measure. To assess if parental support modified relationships between LGBTQ+ status and MH outcomes, additional models (“strengths model” and “feelings model”) interacted support variables and LGBTQ+ status for each outcome.
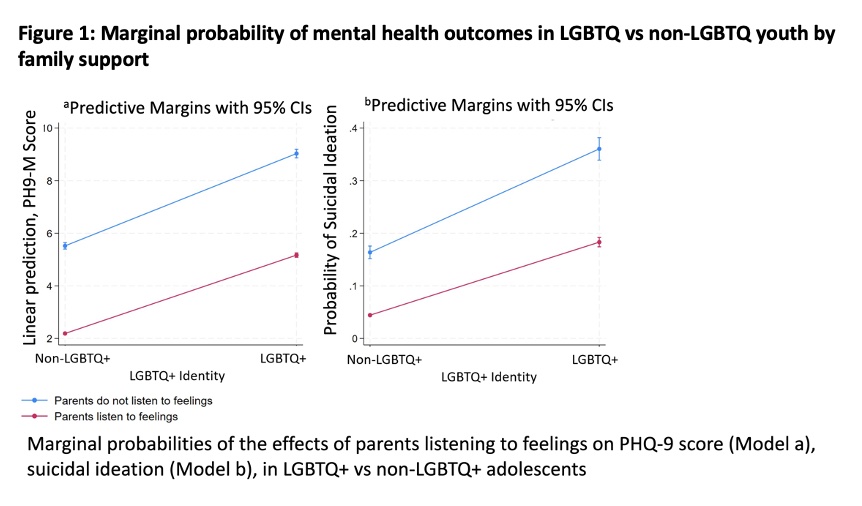
Results: The sample included 60,241 patients. LGBTQ+ youth (16.4% of sample, Table 1), had significantly higher median PHQ-9M scores and higher rates of suicidal ideation. Fewer LGBTQ+ youth endorsed parental support than non-LGBTQ+ youth. In adjusted regression models, LGBTQ+ youth had significantly higher PHQ-9M scores and markedly increased odds of suicidal ideation (aOR 4.73, 95% CI: 4.42,5.05 in strengths model; aOR 4.34, 95% CI: 4.05,4.64 in feelings model, Table 2). For all youth, parental support had a significant protective effect on MH outcomes, including suicidal ideation (aOR 0.46, 95% CI: 0.42,0.50 in strengths model, aOR 0.30, 95% CI: 0.28,0.32 in feelings model). The protective effects of parents listening to feelings were significantly greater in LGBTQ+ compared to non-LGBTQ+ youth for both MH outcomes (Figure 1). For parental discussion of strengths, we identified effect modification for the PHQ-9M score, with stronger protective effects for LGBTQ+ youth.
Conclusion(s): Compared to non-LGBTQ+ youth, LGBTQ+ youth had higher rates of depressive symptoms and suicidal ideation. Youth-reported parental support was protective against these outcomes, suggesting potential MH benefits of family support-focused interventions, particularly for LGBTQ+ youth.
.jpg)