Emergency Medicine
Session: Emergency Medicine 7: Emergency Medical Services
214 - PREVENT: The Pediatric EMS Ventilation Pilot Simulation Trial
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 214
Publication Number: 214.1812
Publication Number: 214.1812

Joseph Finney, MD (he/him/his)
Assistant Professor of Pediatrics
Washington University in St. Louis School of Medicine
SAINT LOUIS, Missouri, United States
Presenting Author(s)
Background: There is an absence of data examining quality of ventilation delivered by emergency medical services (EMS) for pediatric patients in the prehospital setting. The use of a ventilation feedback device (VFD) may improve EMS ability to evaluate pediatric ventilation and improve adherence to accepted ventilation standards.
Objective: 1. To describe quality of EMS-provided pediatric ventilation in a simulated respiratory arrest scenario
2. To evaluate the effectiveness of a VFD to improve adherence to American Heart Association (AHA) ventilation guidelines.
Design/Methods: We conducted a randomized crossover study of EMS from agencies in the St. Louis metropolitan area. Participants completed a simulated pediatric respiratory arrest scenario during which they provided manual ventilation to a toddler mannequin. We recorded tidal volume (TV), respiratory rate (RR), and leakage using a VFD. The VFD can record this data while in unblinded mode and providing real-time feedback to the end-user or capture data in blinded mode without giving feedback.
Participants were randomized to one of two arms. Group 1 completed the scenario unblinded and receiving VFD feedback; Group 2 completed the scenario blinded to VFD feedback. After a 10-minute washout period, groups crossed over and repeated the scenario with blinding status switched. Our primary outcome was proportion of breaths within with AHA recommended parameters. Paired differences between the unblinded and blinded groups were compared using two-tailed Wilcoxon Signed Ranks test.
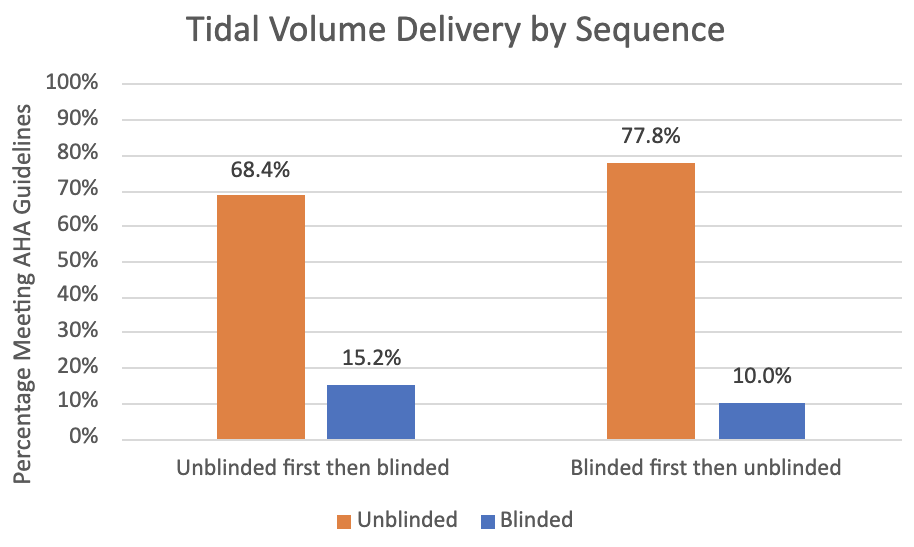
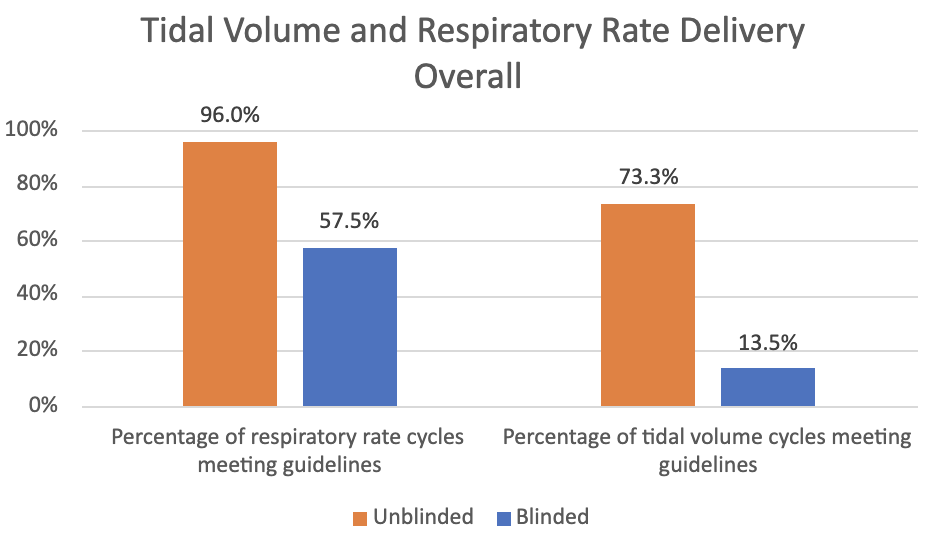
Results: We enrolled 80 participants and 75 were included in analysis. Overall, unblinded participants delivered RR and TV in accordance with AHA guidelines significantly more often than blinded participants (Figure 1, p< 0.001 for both RR and TV). Unblinded participants showed improved ventilation quality regardless of whether unblinded first or second (Figure 2 and 3). The change in ventilation quality from the VFD was lower for participants who were initially unblinded but still statistically significant (p < 0.001). Unblinded participants had significantly lower proportion of cycles with at least 30% leakage compared to blinded participant (10% vs. 21.2%, p=0.02).
Conclusion(s): To our knowledge, this is the first study evaluating pediatric ventilation quality of EMS personnel. Feedback from the VFD significantly improved ventilation quality in our simulation, and its potential impact on clinical care should be evaluated.
.png)