Emergency Medicine
Session: Emergency Medicine 3: Serious Bacterial Infections
90 - Parental Experiences and Preferences for Decision-Making in the Management of their Febrile Young Infant: Insights from a Mixed-Methods Study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 90
Publication Number: 90.1536
Publication Number: 90.1536

Philippe Sylvestre, MD, FRCPC, MSc Student (he/him/his)
MSc Student
Universite de Montreal Faculty of Medicine
Montréal, Quebec, Canada
Presenting Author(s)
Background: Recent guidelines for the management of febrile young infants recommend that when appropriate, decisions regarding lumbar puncture (LP) and hospitalization should incorporate parents’ preferences in a shared decision-making (SDM) process. However, little is known regarding parental preferences for involvement in these decisions, and limited information is available to guide clinicians how to engage in these discussions.
Objective: This study aims to discern parental preferences in SDM concerning the management of their febrile young infant.
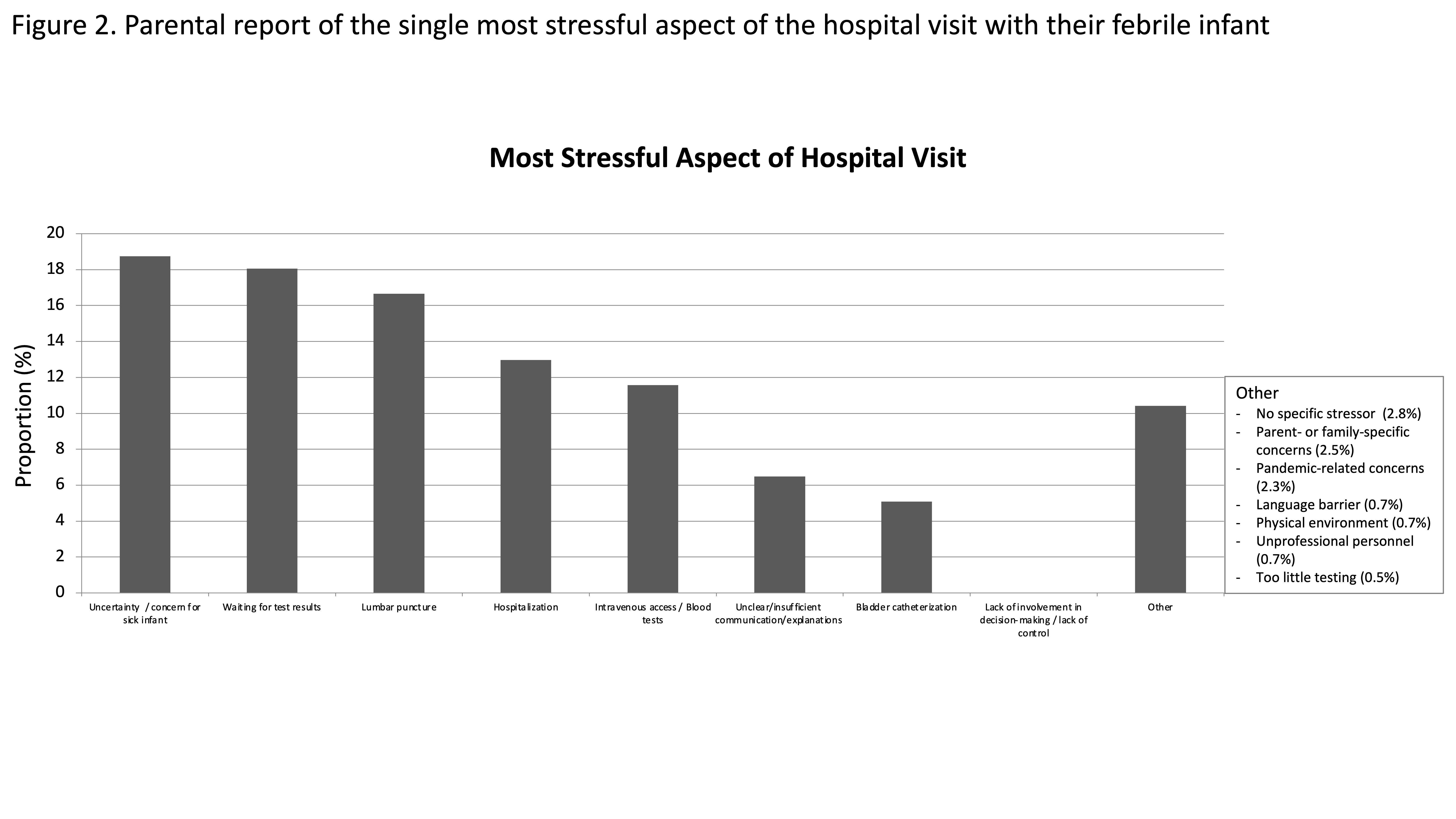
Design/Methods: This was a sequential explanatory mixed-methods study using a cross-sectional questionnaire followed by qualitative focus groups with parents of infants aged ≤60 days evaluated for fever at a tertiary pediatric Emergency Department between May 2020 and May 2022. Parental expectations, stressors, and desired level of decisional involvement were assessed using multiple-choice and 6-point-Likert scales. Questionnaire results informed the qualitative naturalistic inquiry into parents’ decision-making experiences and preferences for LP and hospitalization.
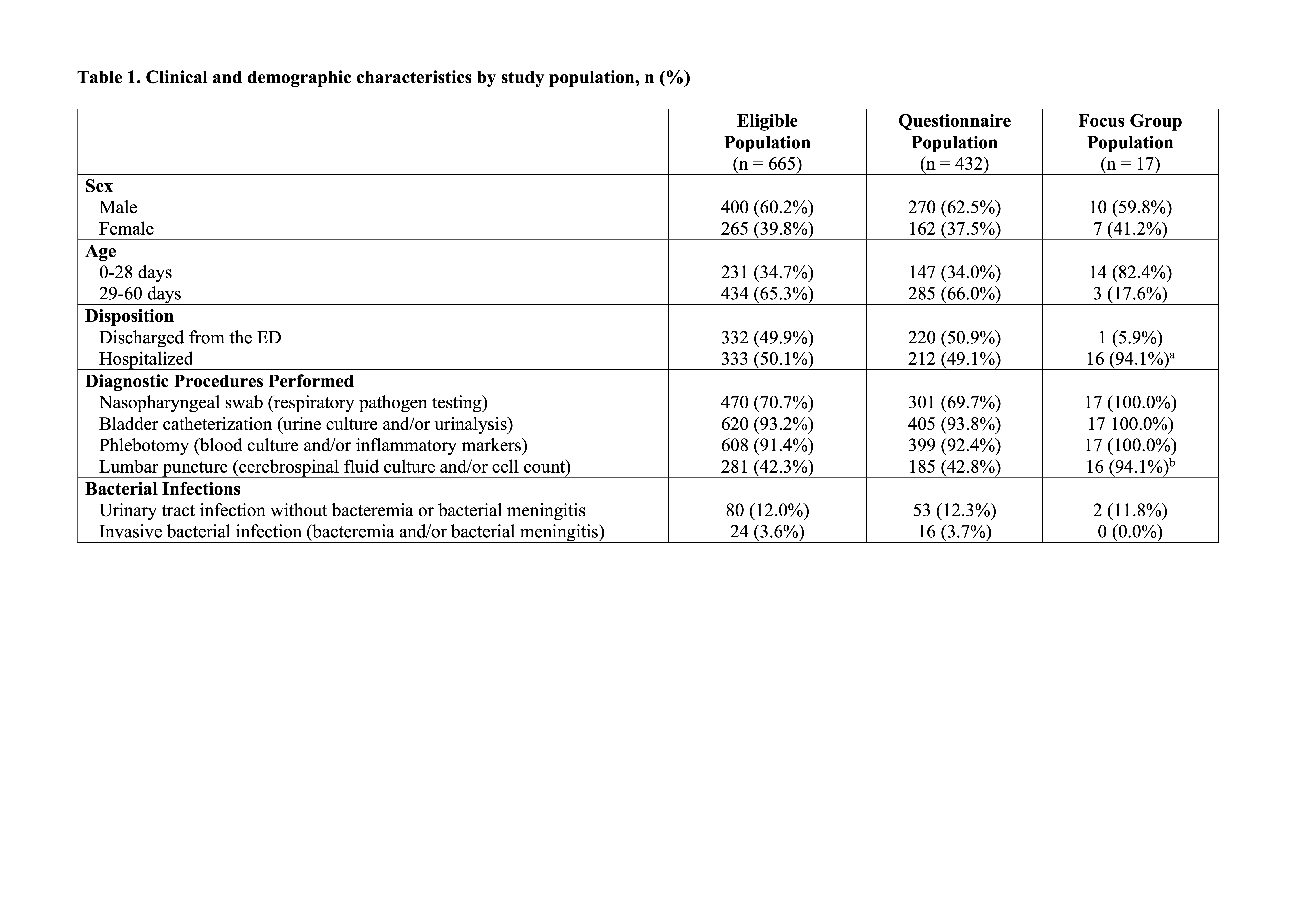
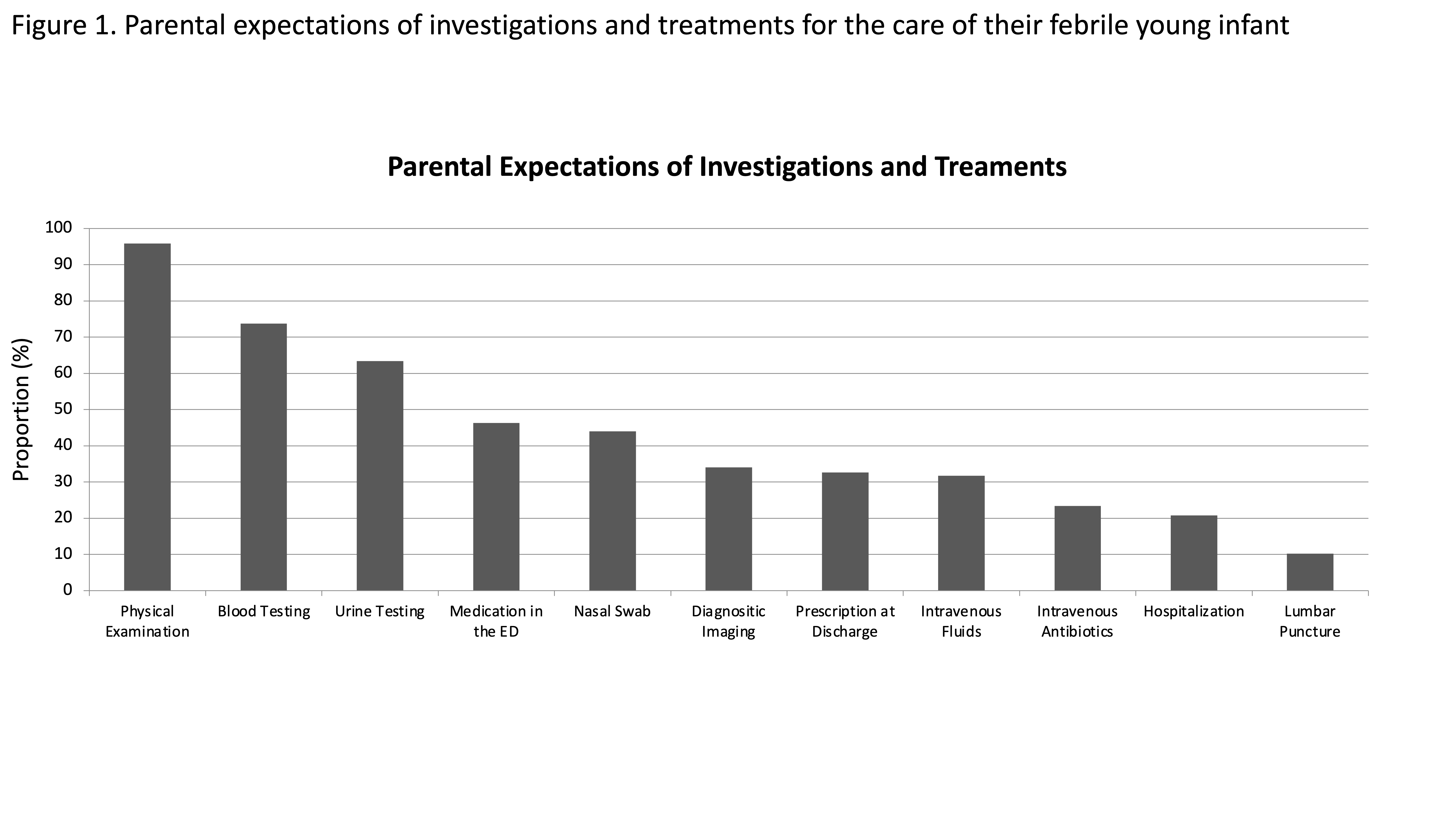
Results: During the 24-month study period, 432/665 eligible families (64.9% response rate) completed post-discharge questionnaires. Few parents anticipated the need for hospitalization (20.8%) or LP (10.2%), and these were selected as the most stressful aspects of management. No family identified lack of decisional involvement as the most important stressor during their visit, though nearly all (97.5%) wanted to be involved in management decisions. Six focus groups with a subset of 17 parents revealed main themes: (1) varying parental preferences for decisional involvement depending on the strength of the medical recommendation; (2) importance of involving parents throughout their child’s ED care; (3) need for tailored information; and (4) importance of supportive relationships. Parents reported that even though decisions regarding LP and hospitalization were usually made by the medical teams, they felt involved in the discussions about their child.
Conclusion(s): In this mixed-methods study involving parents of febrile young infants, LP and hospitalization were the most unexpected and stressful aspects of care. Understanding individual family expectations and tailoring information in relation to the strength of medical recommendation is necessary to guide SDM for febrile young infants.