Hematology/Oncology
Session: Hematology/Oncology
348 - Do you have what it takes to transition? Association of coping strategies and social support on transition readiness among young adults with sickle cell disease.
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 348
Publication Number: 348.121
Publication Number: 348.121
- AI
Apoorva Iyengar, MD (she/her/hers)
Resident
Cohen Children's Medical Center
Manhasset, New York, United States
Presenting Author(s)
Background: Suboptimal preparation of adolescents and young adults (AYA) with Sickle Cell Disease (SCD) from as they transfer from pediatric to adult-care can negatively impact disease outcome, medication adherence, and successful transition to adulthood. Positive coping strategies have been associated with improved transition readiness.
Objective: To evaluate whether coping strategies and social supports in young adults with SCD are associated with transition readiness in a large national sample, and which coping strategies had greatest impact.
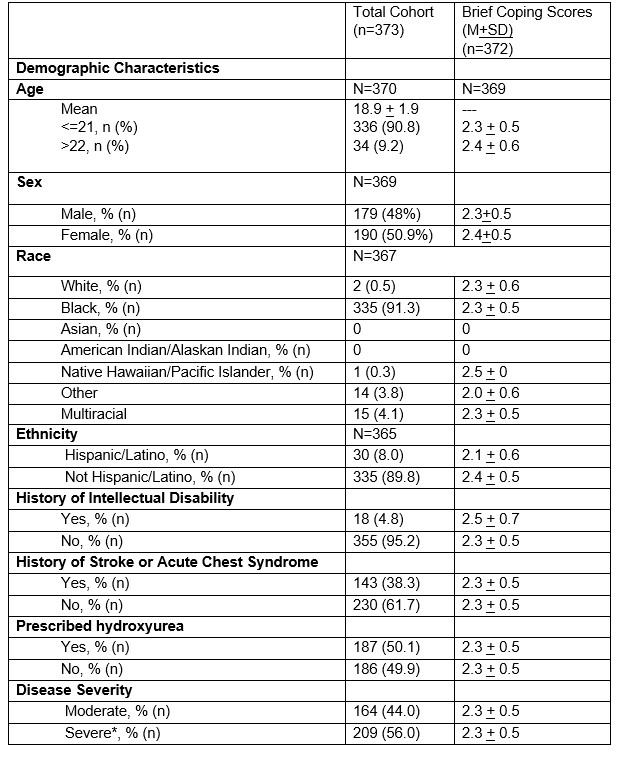
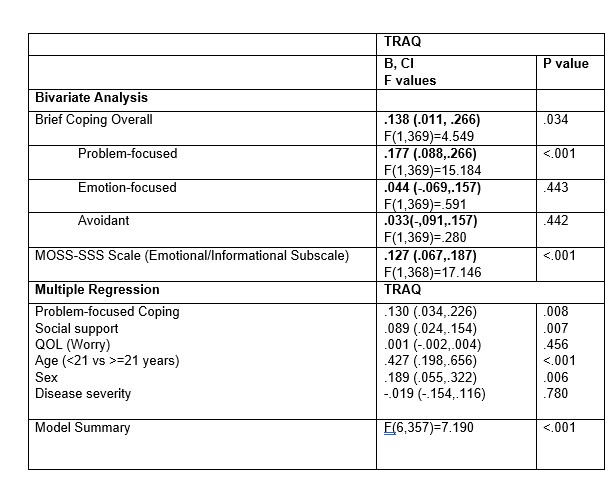
Design/Methods: A retrospective observational study on data collected between 1/2019-12/2022 from AYA with SCD (ages 17-25) planning to transition to adult hematology within 12 months. Data collected from 5 institutions across NY, PA, CT and OH. Outcome was transition readiness, as measured by the Transition Readiness Assessment Questionnaire (TRAQ). Predictors were coping, as measured by Brief COPE (problem focused, emotion focused and avoidant subscales), and social support, as measured by MOS Social Support Survey Emotional/Information Subscale. Multivariate analysis was used to assess the relationship between coping and transition readiness, after adjusting for age, gender, disease severity (acute stroke history, hydroxyurea prescription, hospitalization history), and worry (PedsQL Sickle Cell Module Worry 1).
Results: The 373 participants (Table 1) were equally distributed by gender, largely non-Hispanic black by race/ethnicity, and 56% with severe sickle cell disease. Bivariate analysis showed that overall coping (B=.138, P=0.34) and social support (B=.127, p< 0.001) were significantly associated with transition readiness (Table 2). In particular, problem-focused coping (B=.177, p<.001) was most strongly associated with transition readiness compared to all other coping subscales. After adjusting for age (<=21 vs. >21), gender, disease severity (moderate vs. severe), both coping (b=.130, p=0.008) and social supports (b=0.089, p<.007) were still significantly associated with transition readiness.
Conclusion(s): Targeted behavioral interventions that improve problem-focused coping may be used to improve transition readiness among AYA with chronic disease. Furthermore, interventions that target informational and emotional social supports may further enhance transition readiness among those transitioning to adult care.