Neonatology
Session: Neonatal Pulmonology - Clinical Science 4: Clinical Practice Questions, Going Home
561 - Can Transpyloric feeds play a role in the management of infants with Severe Bronchopulmonary Dysplasia (sBPD)?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 561
Publication Number: 561.3260
Publication Number: 561.3260

Ahana r. Nagarkatti (she/her/hers)
Undergraduate Student, 3rd Year
College of the Holy Cross
W Hartford, Connecticut, United States
Presenting Author(s)
Background: With better prenatal care, antenatal steroids, improved surfactants, and ventilators, smaller and younger babies are surviving. Though the outcomes for Respiratory Distress Syndrome (RDS) have improved, the incidence of severe BPD (sBPD), defined as needing oxygen or positive pressure at 36 weeks corrected gestational age (CGA) has remained the same. Diuretics, steroids and specialized ventilator settings have been standard of care for these infants who are at very high risk for developing lethal pulmonary hypertension (PPHN) or needing surgical interventions such as Gastrostomy Tubes (GT) for nutrition or Tracheostomies for pulmonary support. The finding of pepsin in the lungs of extremely low birth weight (ELBW < 1000g) infants with sBPD has led to the speculation that gastroesophageal reflux (GER) and aspiration could contribute to their lung disease, but micro-aspiration-reducing strategies such as Transpyloric feeds (TP) have not been well studied.
Objective: 1. Compare ELBW infants with sBPD managed with or without TP feeds and determine the difference between the 2 groups for illness severity, late PPHN & need for GT, 2. Evaluate the change in respiratory support before and after the initiation of TP feeds
Design/Methods: Retrospective study based on ELBW admissions to the CCMC NICU between Jan 2010 - June 2023. ELBW survivors to 36-wk CGA were included. Infants with GI pathology, death, or transfer < 36 wks CGA were excluded. Data for demographics, sBPD morbidities, details of TP feeds, medications, and length of stay were gathered from the EPIC database. SPSS software was used for X2, Mann-Whitney U and unpaired T-tests as appropriate.
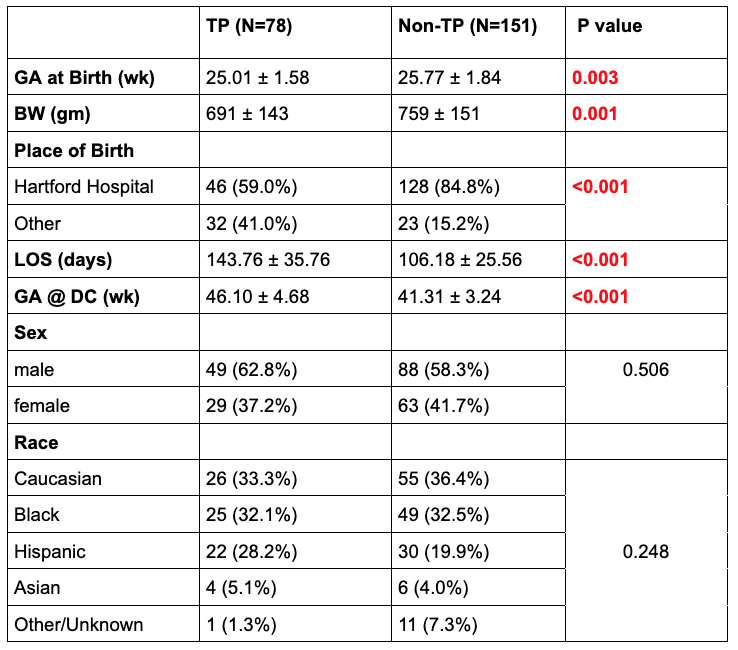
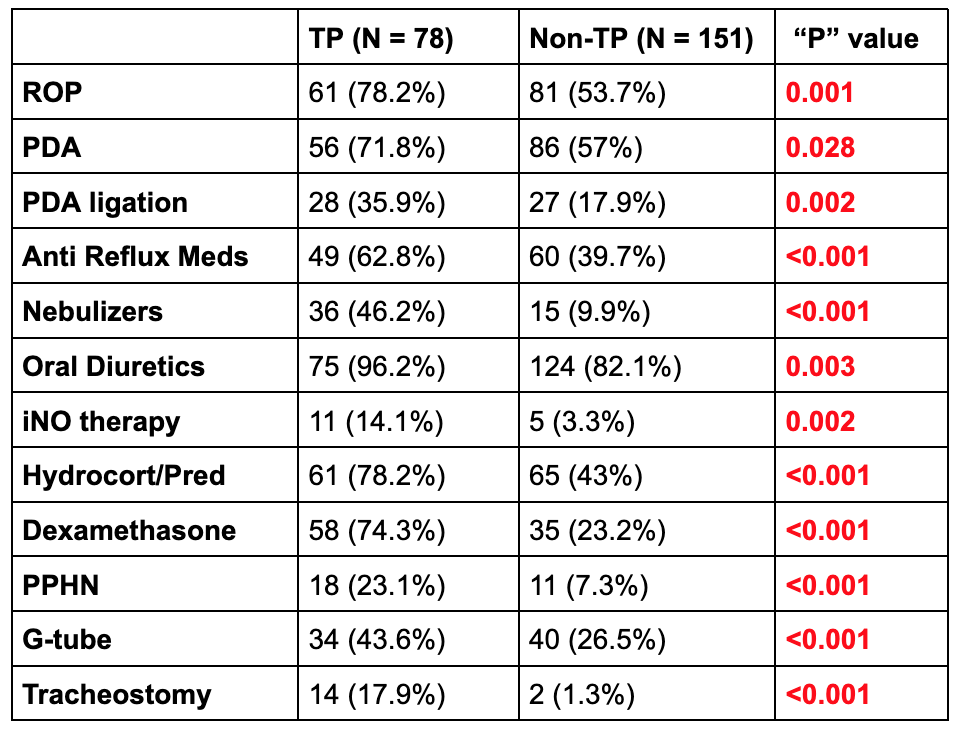
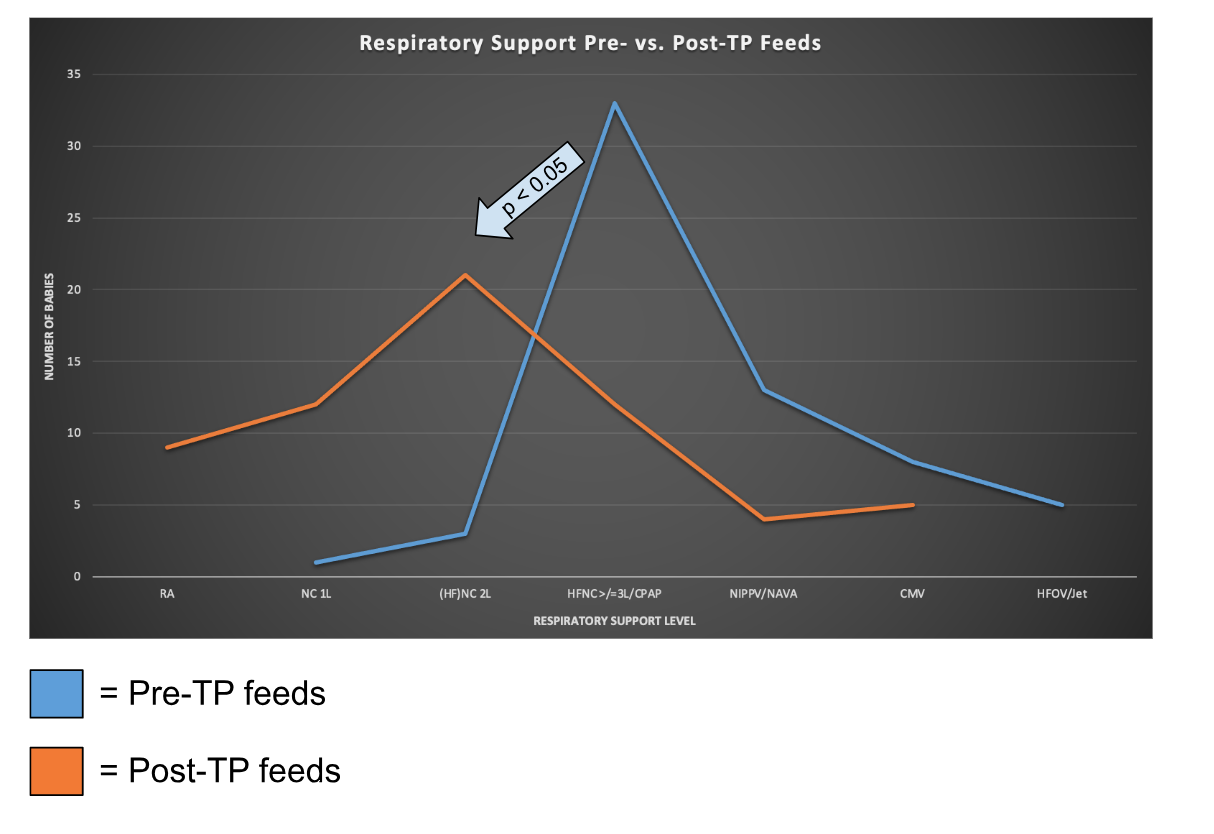
Results: 229 ELBW sBPD infants in the study (78 in the TP study group and 151 in the non-TP control group). Though there was no difference in the sex or race among the two groups, the following were significant in the TP group compared to the non-TP group (Table 1): 1. The TP group had lower BW and GA and a higher severity of illness at initiating TP feeds based on known morbidities or the use of medications (Table 1&2), 2. TP group had a higher incidence of late PPHN & 3. higher need for G-tubes (Table 2). Also, in pre-post analysis within the TP group, the need for respiratory support (based on respiratory score) decreased significantly after the initiation of TP feeds (Graph 1).
Conclusion(s): TP was more frequently used in the sicker & younger ELBW infants, there was a significant improvement in respiratory severity score after its initiation. TP feeds could play an important role in the management of ELBW infants with sBPD. Prospective studies are needed.