Emergency Medicine
Session: Emergency Medicine 8: Mental Health
582 - Mental Health Resources for Patients with Prior Suicidality: An Emergency Department Initiative for Safe Discharge Planning
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 582
Publication Number: 582.1723
Publication Number: 582.1723

Sarah Benett, MD (she/her/hers)
Resident Physician
Johns Hopkins Children's Center
Baltimore, Maryland, United States
Presenting Author(s)
Background: Suicide is the second leading cause of death amongst adolescents in the United States. More than 60% of suicide completions involve recent medical system contact, including emergency department (ED) visits. This QI initiative occurred in an urban academic pediatric ED with 36,000 annual visits. All patients over 10 years of age are universally screened for suicidal ideation, however, there is no standard practice for distributing mental health resources to patients who present with primarily medical concerns and are found to screen positive for suicidal ideation and are determined to be low risk for suicide.
Objective: We aimed to increase the proportion of After Visit Summaries (AVS) containing mental health resources for medical patients who were identified as having non-acute suicidal ideation, at low risk of suicide, and discharged from the pediatric ED by 25% within 6 months.
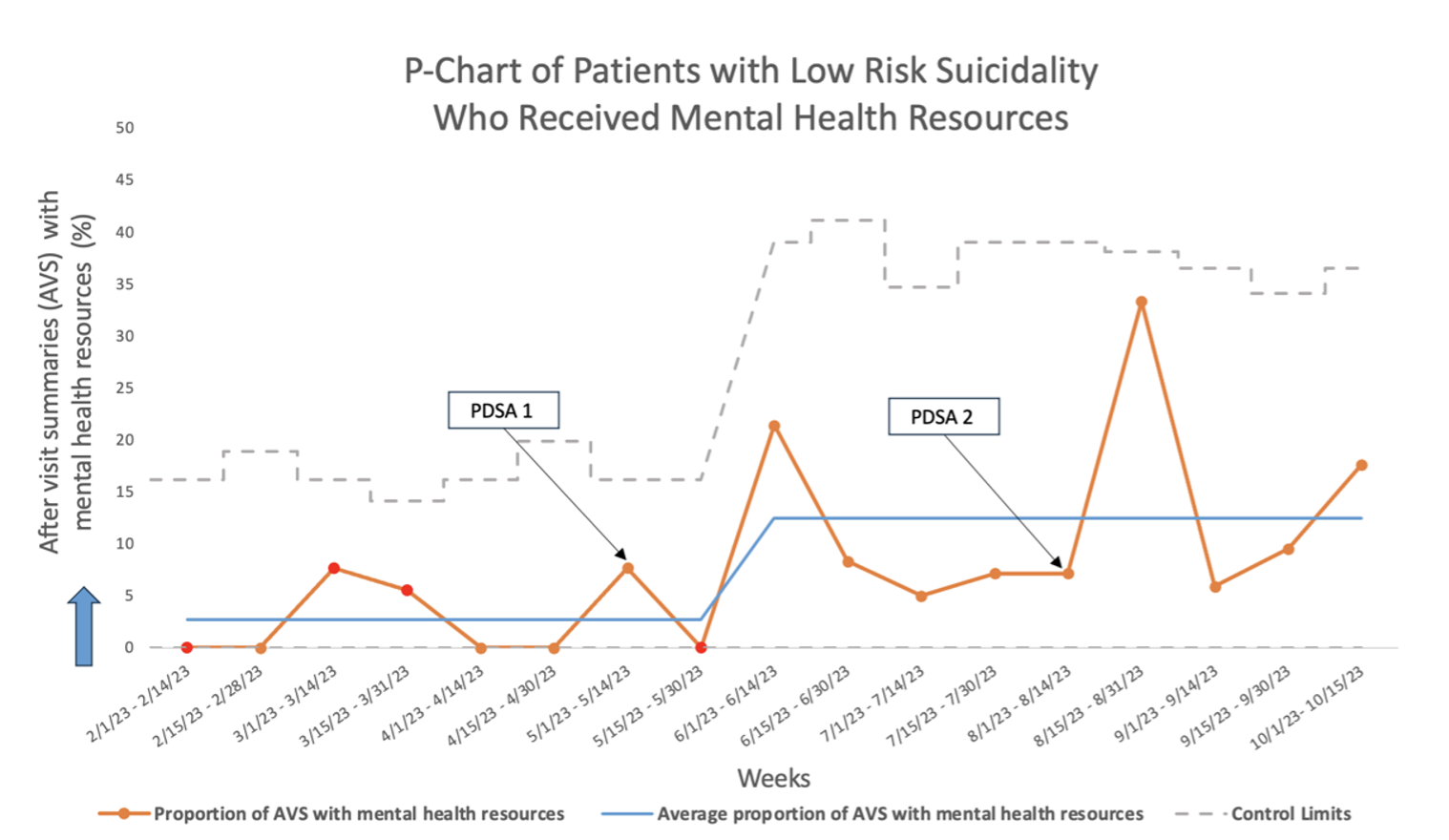
Design/Methods: A multidisciplinary team targeted the following key drivers: 1) multidisciplinary engagement 2) training and education of providers and 3) health information technology. Plan-Do-Study-Act cycles included 1) an educational campaign with regular multidisciplinary meetings, educational updates, and email reminders; and 2) electronic health record changes. The primary outcome measure was the proportion of discharged medical patients who screened positive for suicidal ideation and were determined to be at low risk for suicide who received mental health resources on discharge. We analyzed data using statistical process control.
Results: The proportion of AVS containing mental health resources for the target population increased from 2.7% to 12.5% within 5 months, with electronic health record system change offering higher gains in the percentage of patients receiving mental health resources compared with educational interventions. There was a special cause variation associated with PDSA cycles.
Conclusion(s): This QI project demonstrated improvement in mental health resource distribution within the pediatric ED for low-risk suicidality medical patients. By continuing to expand this initiative, we aim to provide mental health resources to all patients who screen positive for suicidal ideation.