Neonatology
Session: Neonatal Neurology 5: Clinical
539 - The Reference of Cerebral Blood Flow in Extremely Preterm Infants: A Study Utilizing Multidiscipline Cerebral Hemodynamic Monitors
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 539
Publication Number: 539.1322
Publication Number: 539.1322

Wei-Hung Wu, MD
fellowship
Chang Gung Memorial Hospital, Linkou branch
Taoyuan, Taoyuan, Taiwan (Republic of China)
Presenting Author(s)
Background: Cerebral blood flow (CBF) has a pivotal role in cerebral hemodynamics. Maintaining normal CBF by avoiding hypo- or hyper- cerebral perfusion is critical for extremely preterm infants to prevent neurologic complication. However, there is a lack of comprehensive definition for normal CBF and no suggestive reference in extremely preterm infants. With the advance of non-invasive hemodynamic monitors, we may have an opportunity to define normal cerebral hemodynamics.
Objective: This study aimed to establish a reference range of CBF in extremely preterm infants of varied age and weight.
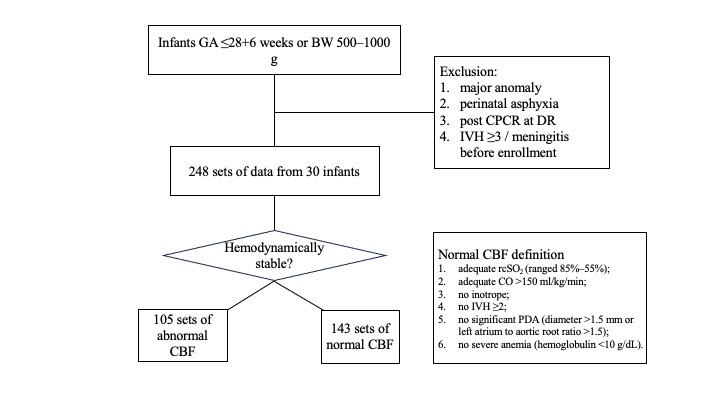
Design/Methods: This prospective study encompasses various hemodynamic monitors and focuses on preterm infants with gestational age (GA) of ≤28 weeks or birth weight (BW) ≤1000 g. Infants with significant anomaly, perinatal asphyxia or post resuscitation were excluded. Multiple monitors, which included near-infrared spectroscopy (NIRS), electrical cardiometry (EC), brain functional echography (fEcho) to measure CBF and screen IVH, and cardiac fEcho to screen patent ductus arteriosus (PDA). The monitoring protocol consisted of continuous NIRS+EC plus daily fEcho within the first 72 hours of life, followed by weekly assessments in the first month and monthly assessments until discharge or term-equivalent age. Parameters to evaluate CBF included peak systolic velocity (PSV), end diastolic velocity (EDV), mean velocity (MV), pulsatile index (PI) and resistance index (RI). To establish the definition of normal CBF, this study employed a set of criteria to be met: (1) adequate rcSO2 (ranged 85%–55%); (2) cardiac output (CO) >150 ml/kg/min; (3) without inotrope; (4) no IVH ≥2; (5) no significant PDA (diameter >1.5 mm or left atrium to aortic root ratio >1.5); (6) no severe anemia (hemoglobulin < 10 g/dL) (Fig 1).
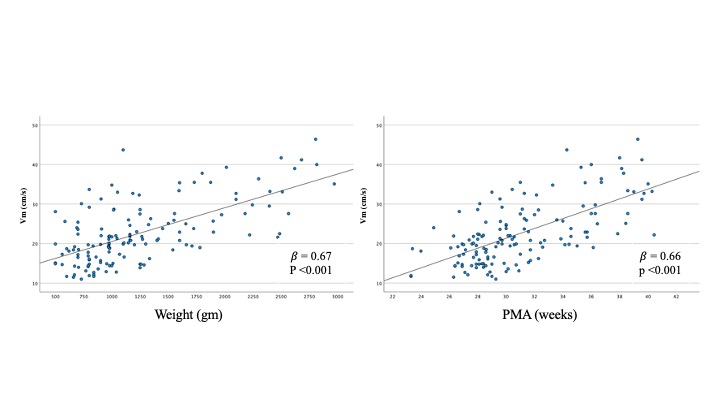
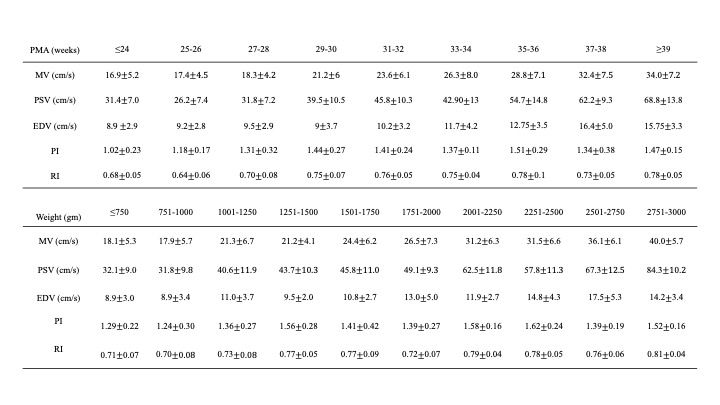
Results: A total of 30 extremely preterm infants (GA 27.1±2.0 weeks, BW 830±225 g) were enrolled, and 138 CBF datasets were in normal hemodynamic status. Strong correlations were seen between CBF velocities (PSV, EDV, MV) and post-menstrual age (PMA) or weight (Fig 2). Consequently, we proposed reference ranges for PSV, EDV, MV, PI and RI according to PMA or weight (Table 1). Our findings also found MV remained independent to mean blood pressure or CO (ml/kg/min), indicating preserved cerebral autoregulation.
Conclusion(s): By employing multidiscipline cerebral hemodynamic monitors to define normal CBF, a reference range of CBF was suggested in extremely preterm infants.