Neonatology
Session: Neonatal Neurology 3: Clinical
36 - Early versus Late Brain Magnetic Resonance Imaging and Spectroscopy in Infants with Neonatal Encephalopathy
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 36
Publication Number: 36.596
Publication Number: 36.596
.jpg)
Tatiana A. Nuzum, MB BCh BAO (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: Magnetic Resonance (MR) Imaging is the current gold standard for early neurodevelopmental prognostication of infants with Neonatal Encephalopathy (NE). Recent studies have suggested that obtaining MR imaging (MRI) at a single time-point may underestimate the degree of neurologic injury. MR Spectroscopy (MRS) is a newer modality of neuroimaging that may be more sensitive in the detection of hypoxic-ischemic injury.
Objective: To evaluate the utility of early and late MRI in infants with NE, and to determine the concordance between MRS and initial MRI.
Design/Methods: This was a retrospective chart review including infants with NE born between 2017 and 2023 at two regional perinatal centers, NYU Langone Health and Bellevue Hospital Centers. Demographic and clinical information including MRI results were collected. All infants underwent early diffusion-weighted MRI with MRS, and late conventional T1/T2-weighted imaging.
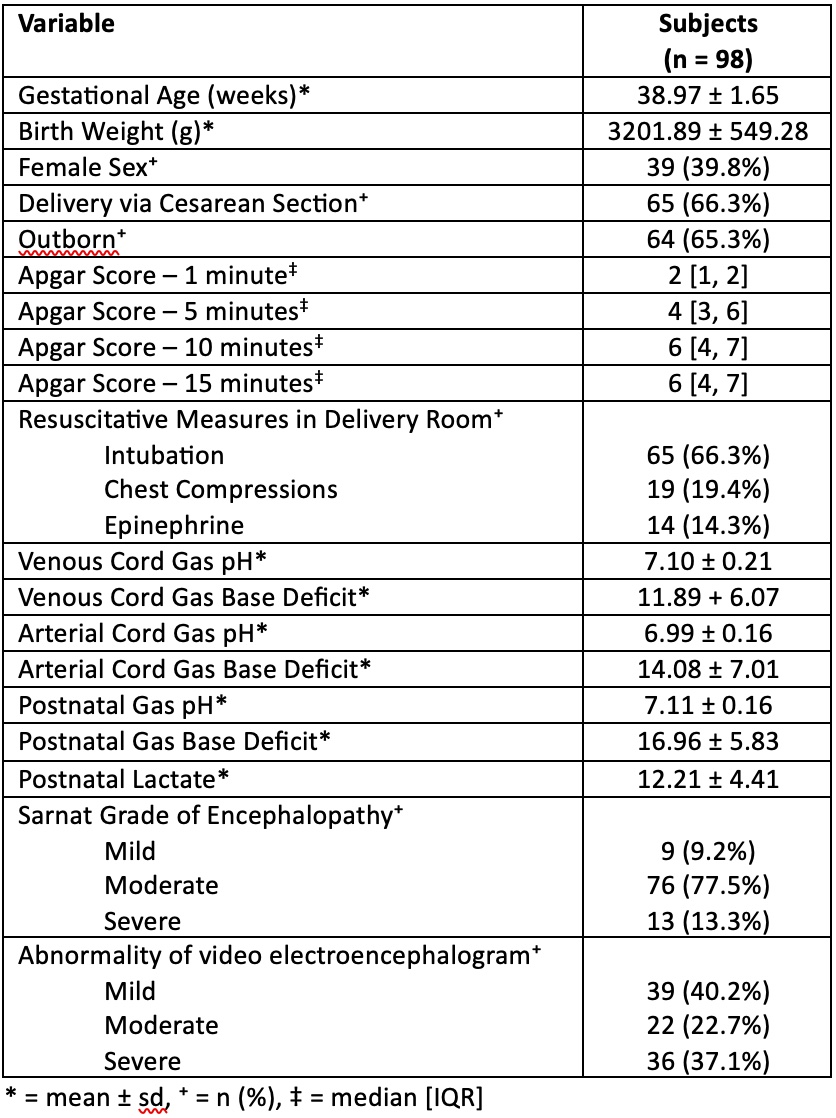
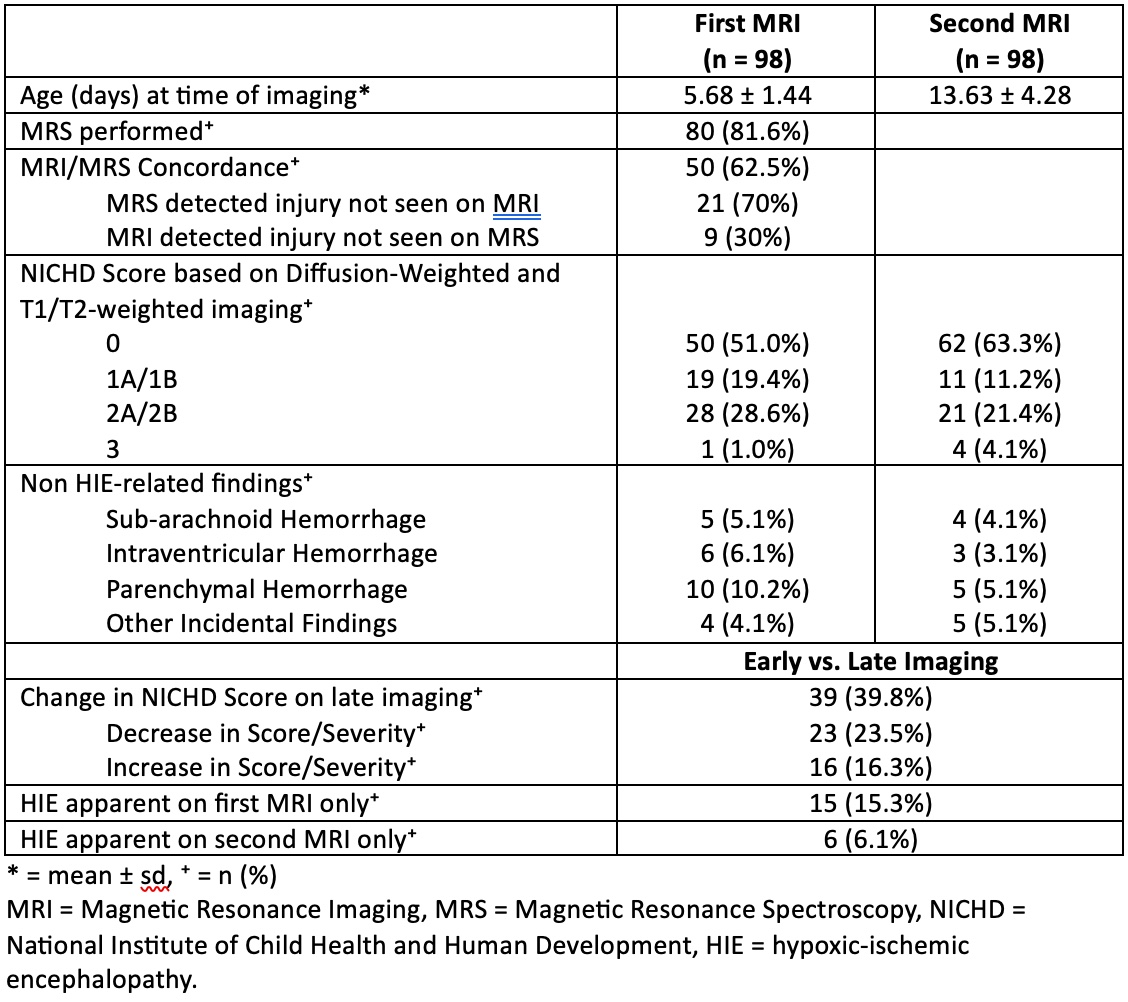
Results: Ninety-eight infants were included. Subject demographics are described in Table 1. The majority (78%) were moderately encephalopathic. Early and late MR imaging was performed at an average of 5.7 and 13.6 days of life respectively. Both MRIs were assigned an injury severity score based on the NICHD NRN pattern of injury. Differences in these scores between first and second MRIs are outlined in Table 2. Forty percent of infants exhibited a change in severity of injury between early and late MRI. Twenty-three infants (24%) were found to have milder injury and 16 (16%) were found to have more severe injury according to late imaging. Fifteen percent of infants had evidence of hypoxic-ischemic injury on early imaging only, and 6% on late imaging only. Eighty infants (82%) underwent MRS with early imaging. Concordance of injury severity between MRS and MRI was 62.5%. Among the cases of discordant MRI/MRS, MRS detected additional injury in 70% of cases, and MRI detected additional injury in 30% of cases. MRI findings unrelated to hypoxic-ischemic injury are also outlined in Table 2.
Conclusion(s): Both early and late imaging are necessary to fully define neurologic injury and provide accurate neurodevelopmental prognoses in cases of neonatal encephalopathy. Had imaging not been performed at two intervals, radiologic diagnoses of hypoxic-ischemic injury would have been missed in 6-15% of cases, and characterization of injury may have been inaccurate in up to 40% of cases. Further analysis of MRS results with an independent reviewer may test the superiority of this modality in comparison to conventional MR imaging, given the discrepancy found in this study.