Neonatology
Session: Neonatal General 6: POCUS, Technology in NICU
152 - Feasibility Of Using Ultrasound To Improve Lumbar Puncture Success Rate In Neonates By Physicians Without Prior Ultrasound Experience
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 152
Publication Number: 152.2114
Publication Number: 152.2114
- AY
Amy Yeh, MD, MPH
Keck School of Medicine of the University of Southern California
Los Angeles, California, United States
Presenting Author(s)
Background: Even though lumbar puncture (LP) is one of the most common procedures performed in the neonatal intensive care unit (NICU), failure rate is reported to be as high as 30-50%. Traditionally, LP has been performed with palpation of landmarks; however, there are emerging data that describe the use of ultrasound (US) by US trained physicians to improve success rate of LP by either marking the area of interest prior to insertion of the needle (static) or to guide LP in real time (dynamic). The success rate and rate of traumatic puncture of US guided LP performed by physicians without any prior ultrasound experience is not known.
Objective: The objective of this study is to assess the feasibility of dynamic and static US guided LPs by physicians without prior US training and to determine if using US to guide LP improve success rate.
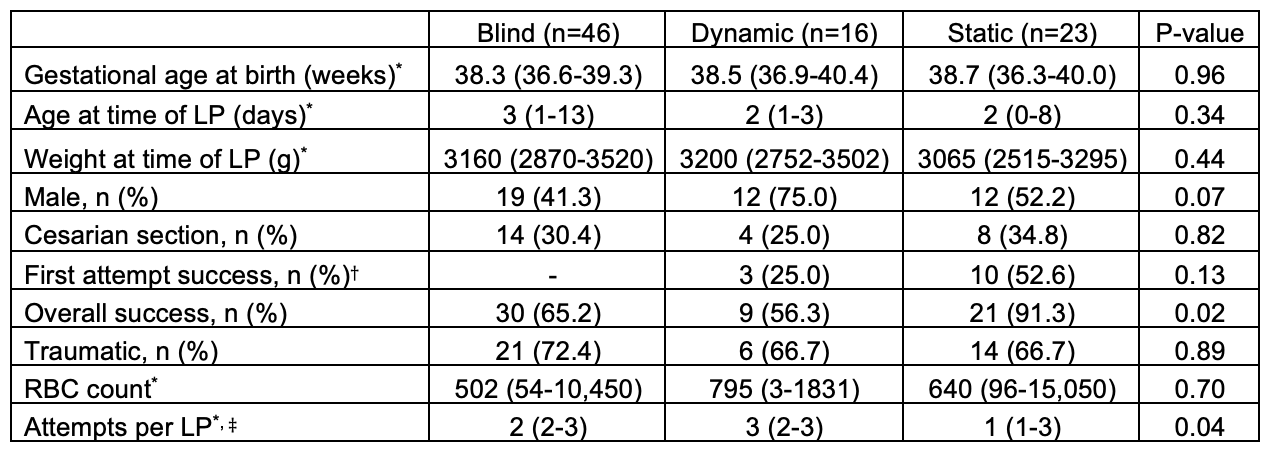
Design/Methods: Neonates admitted to the NICU at Los Angeles General Medical Center starting in May 2021 who required LPs were included in the study. Prior to May 2022, all LPs were performed with landmark (blind) technique and starting in May 2022, US guided LP became routine practice and training was provided prior to the procedure. US guided LPs were initially performed with dynamic technique, but the static technique was introduced to compare success rate. Successful LP was determined when CSF was obtained. Traumatic puncture was defined as presence of red blood cells (RBC) greater than 10,000/mm3 in the CSF. Outcomes of LP performed with the three techniques, landmark, static, and dynamic, were compared.
Results: 85 neonates were included in the study. Mean birth gestation age was 37.7 ± 3.1 weeks and mean weight was 3,040 ± 819 grams at the time of LP. There was significant improvement in the overall LP success rate and decrease in the number of attempts per LP when performed by US guided static technique. There was no significant improvement in first attempt success rate with static LPs compared to dynamic LPs; blind LPs were not compared in the analysis due to incomplete documentation. There was no difference in the traumatic rate between the LPs performed by the three techniques (Table).
Conclusion(s): Our study demonstrated that static US guided technique to assist LP by marking the area of interest prior to insertion of LP needle is feasible in physicians without prior ultrasound training with improved success rate and decrease in the number of attempts performed. However, dynamic US guided LP may be more difficult in physicians with no prior US experience compared to static US guided LP.